Experiencing bad breath can be an embarrassing and often uncomfortable issue to discuss. Despite the effectiveness of large mouthwash industries, public concern continues as many mouthwashes do not significantly impact bad breath. Understanding this phenomenon begins with categorizing bad breath into genuine halitosis, pseudo-halitosis, and halitophobia.
Understanding the Problem
Genuine halitosis is actual bad breath, pseudo-halitosis is when the perception of bad breath is not reflective of true malodor, and halitophobia is the fear of having bad breath despite the absence of it. Oral sources of bad breath often stem from bacteria that produce odor-causing compounds found in gum disease or on the tongue. Non-oral sources can include medical conditions like diabetes, gastrointestinal issues, and certain diets.
Can Dental Crowns Cause Bad Breath?
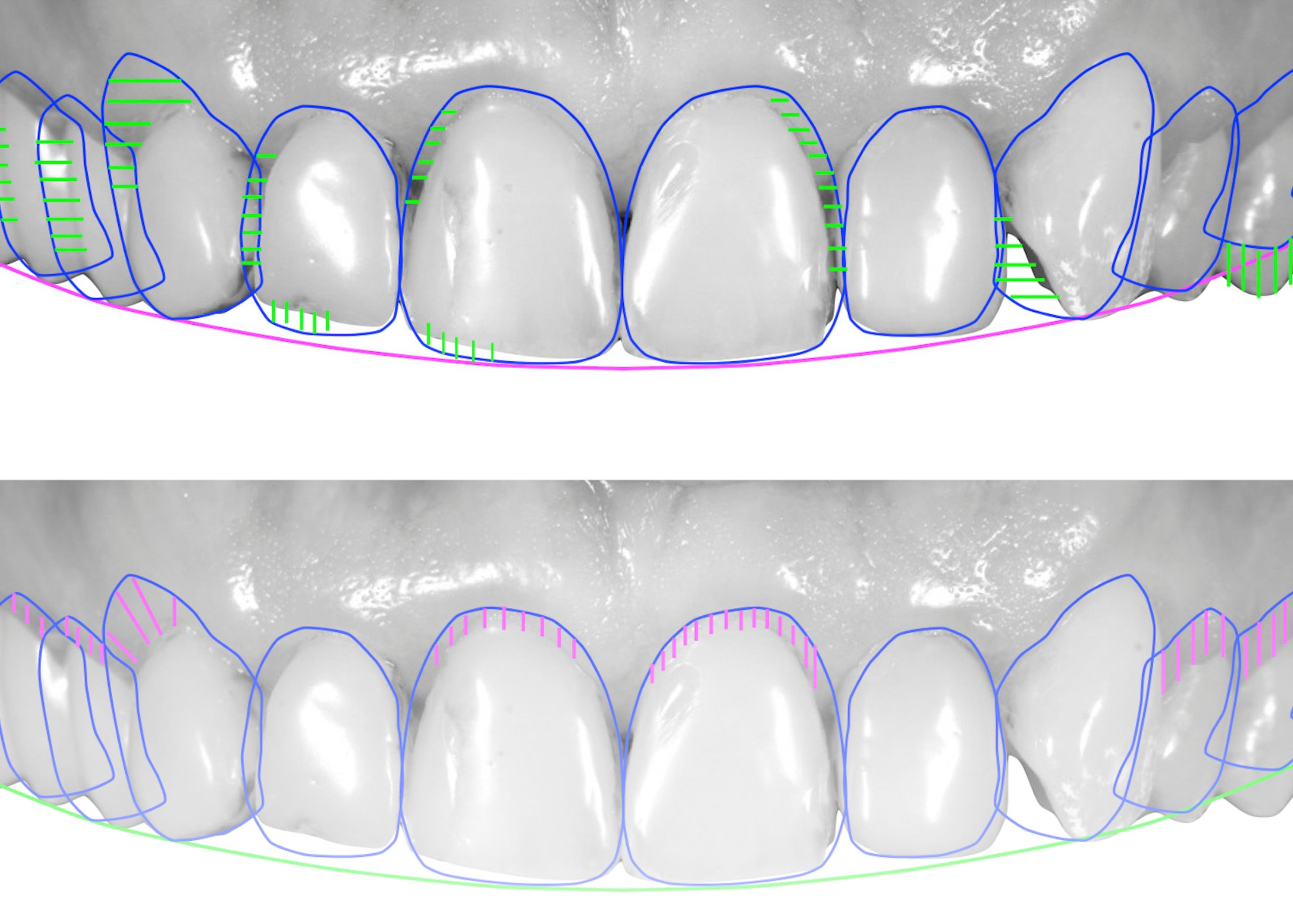
While dental crowns themselves do not directly cause bad breath, the installation process and the materials used may temporarily affect saliva flow, leading to dry mouth—a condition that can exacerbate bad breath. Properly fitted and well-maintained dental crowns should not contribute to bad breath and can even help improve oral health when replacing damaged teeth.
Management and Prevention
Effective management of bad breath involves a combination of improved oral hygiene and professional dental care:
- Enhance Oral Hygiene: Effective home care routines such as regular tooth brushing, flossing, and the use of a water flosser can significantly reduce halitosis. Brushing or scraping the tongue to remove bacteria is also recommended.
- Regular Dental Check-Ups: Ensure your dental crowns are properly fitted and address any oral health issues promptly. Regular cleanings can control gum disease and minimize bacteria.
- Care for Removable Appliances: For those with removable dentures, ensure they are cleaned after each meal and avoid wearing them during sleep to prevent bacterial growth.
- Simple Home Remedies: Decreasing the intake of odor-inducing foods like onions and garlic, rinsing with salt water, and staying hydrated can also help manage bad breath.
Conclusion
Maintaining excellent oral hygiene and regular dental visits are crucial for managing bad breath. Overuse of certain mouth rinses can dry out the mouth, exacerbating bad breath, as can lifestyle factors like smoking and alcohol consumption. Proper hydration is essential for keeping the mouth fresh.
Final Thought: Do Dental Crowns Cause Bad Breath?
Dental crowns do not directly cause bad breath; however, poor installation and inadequate oral hygiene can lead to issues. Open communication with your dentist about material concerns and regular hygiene practices are key to preventing bad breath.