The landscape of modern surgery has undergone a remarkable transformation. Minimally invasive surgery has revolutionized healthcare, offering patients safer, more precise procedures with significantly faster recovery times. At Burjeel Medical City, Abu Dhabi, our expert laparoscopic surgeons are at the forefront of this medical revolution, providing cutting-edge minimally invasive treatments that prioritize patient comfort and optimal outcomes.
Whether performed through advanced laparoscopic surgery techniques or with state-of-the-art robotic assistance, minimally invasive surgery has become the gold standard for treating numerous medical conditions. This comprehensive guide explores everything patients need to know about these revolutionary surgical approaches.
What is Minimally Invasive Surgery?
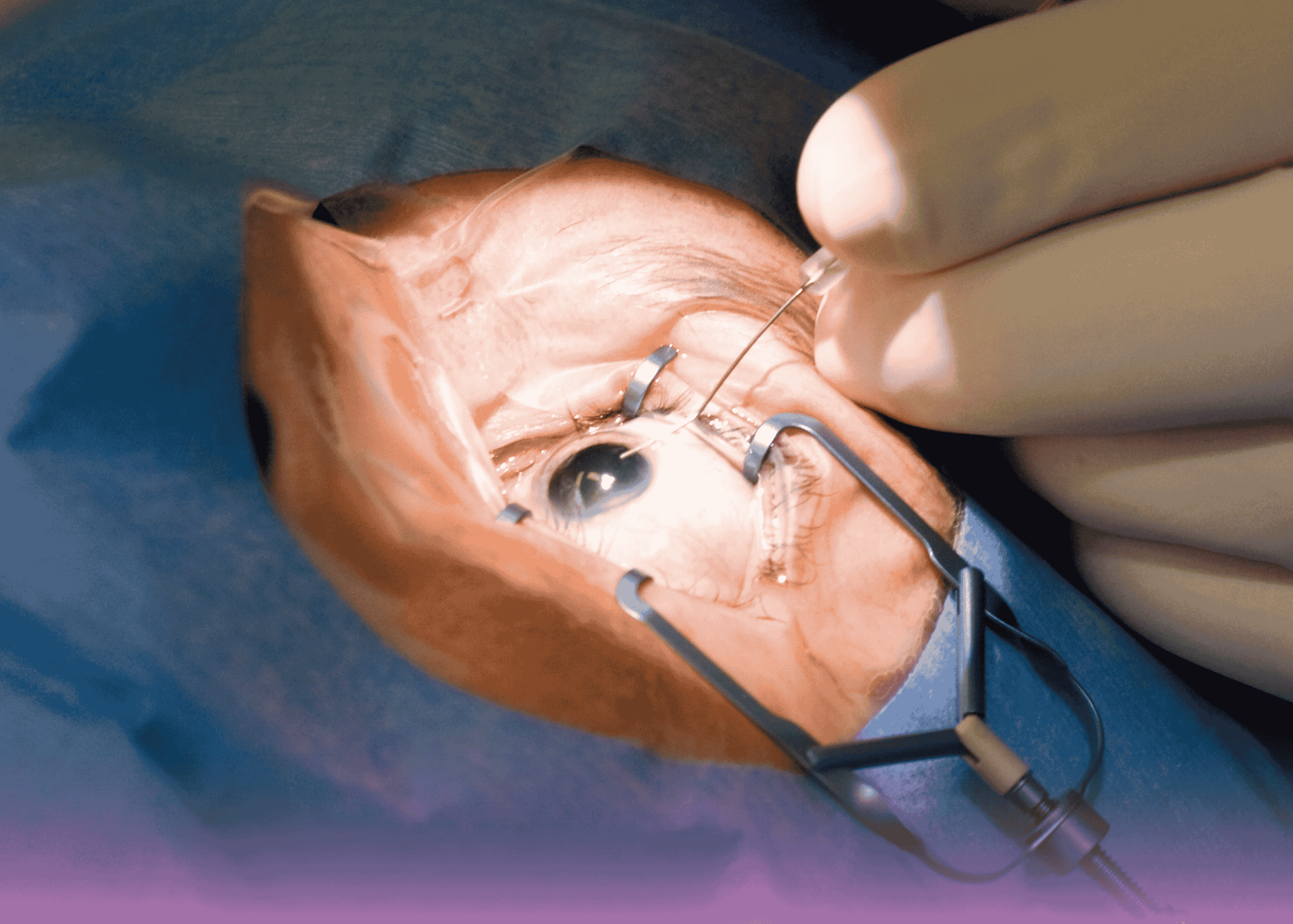
Minimally invasive surgery represents a paradigm shift from traditional open surgical procedures. Instead of creating large incisions that require extensive tissue disruption, minimally invasive surgery utilizes small, strategically placed incisions through which specialized instruments and cameras can access the surgical site.
This innovative approach allows general and laparoscopic surgeons to perform complex procedures with unprecedented precision while minimizing trauma to surrounding healthy tissues. The result is a surgical experience that prioritizes patient comfort, safety, and rapid recovery.
Core Components of Minimally Invasive Surgery
Laparoscopic surgery forms the foundation of most minimally invasive treatments. This technique employs:
- Advanced Imaging Technology: High-definition cameras provide surgeons with detailed, magnified views of internal structures
- Specialized Instruments: Precision tools designed specifically for laparoscopic surgery allow for delicate tissue manipulation
- Small Access Points: Tiny incisions, typically measuring just 0.5 to 1.5 centimeters, serve as entry points for surgical instruments
Types of Minimally Invasive Surgery
Laparoscopic Surgery: The Gold Standard
Laparoscopic surgery utilizes a thin, flexible tube equipped with a high-definition camera (laparoscope) and specialized surgical instruments. Our experienced laparoscopic surgeons insert these tools through small incisions, allowing for precise surgical intervention with minimal tissue disruption.
The benefits of minimally invasive surgery include:
- Superior visualization of internal structures
- Enhanced precision during complex procedures
- Minimal scarring and improved cosmetic outcomes
Robotic-Assisted Surgery: The Next Evolution
Building upon traditional minimally invasive techniques, robotic-assisted procedures represent the cutting edge of laparoscopic surgery. This advanced approach combines the benefits of laparoscopic surgery with enhanced technological capabilities:
- Enhanced Dexterity: Robotic arms provide laparoscopic experts with greater range of motion and precision
- 3D High-Definition Visualization: Superior imaging technology offers unprecedented detail and depth perception
- Improved Ergonomics: Reduced surgeon fatigue allows for more consistent performance during lengthy procedures
Common Applications of Minimally Invasive Treatments
At Burjeel Medical City, our leading laparoscopic surgeons utilize minimally invasive surgery techniques across a wide range of medical specialties:
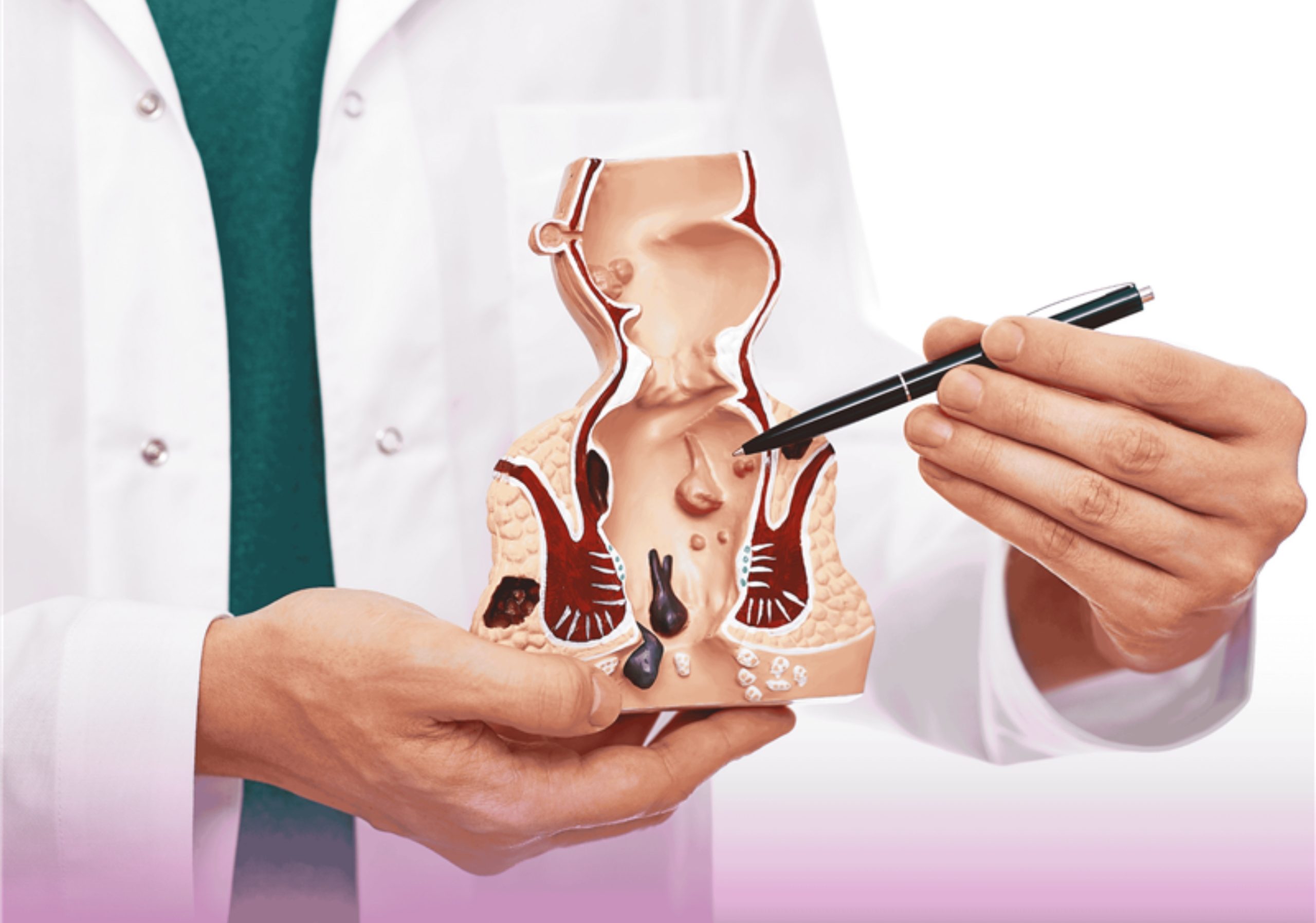
Gastrointestinal Procedures
- Laparoscopic Cholecystectomy: Gallbladder removal using minimally invasive surgery techniques
- Appendectomy: Laparoscopic surgery for appendix removal with faster recovery times
- Colon Surgery: Advanced minimally invasive treatments for colorectal conditions and cancer
General Surgery Applications
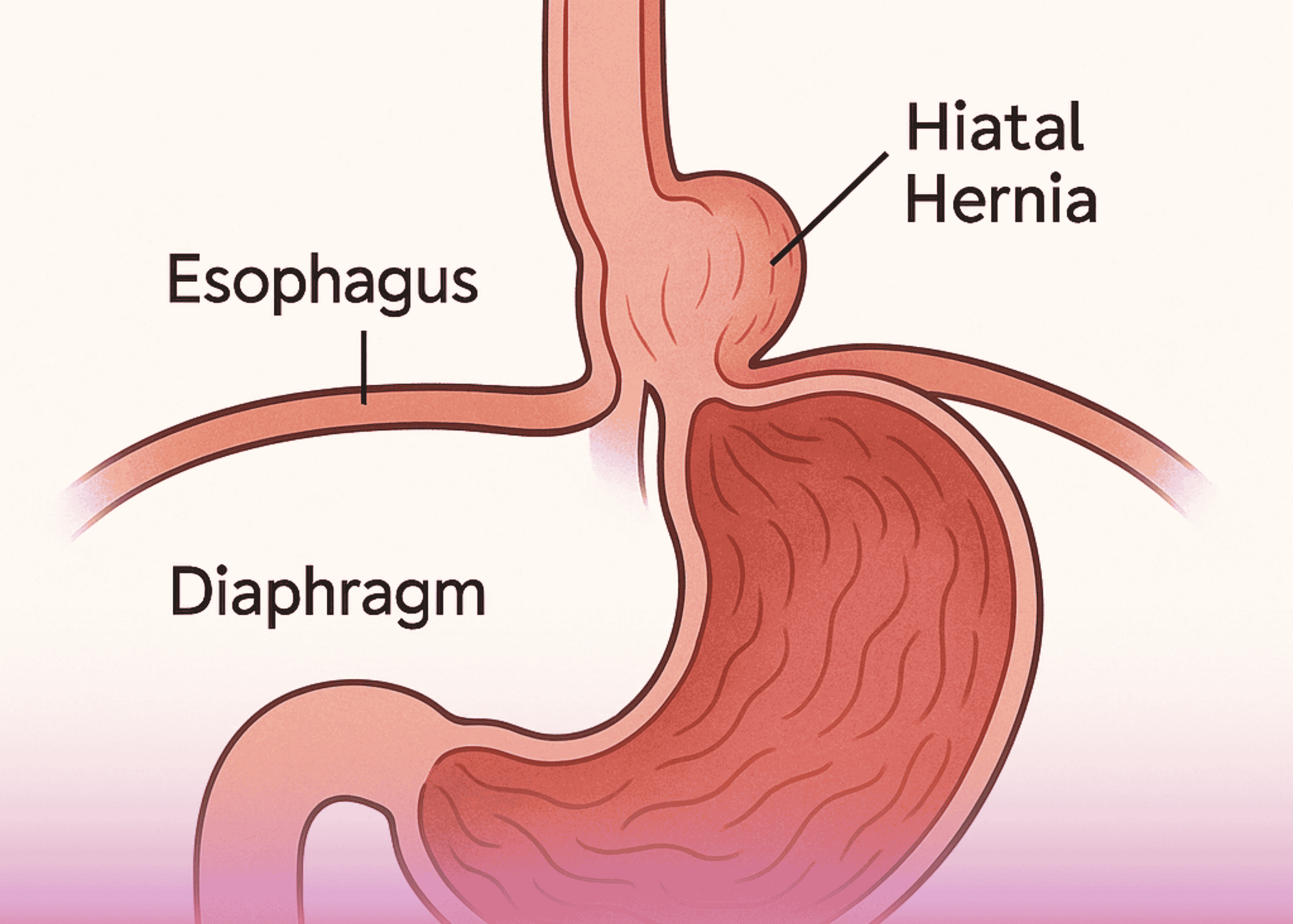
- Hernia Repair: Laparoscopic surgery approaches for various types of hernias
- Bariatric Surgery: Minimally invasive treatments for weight management and metabolic disorders
- Anti-Reflux Procedures: Laparoscopic surgery solutions for gastroesophageal reflux disease
Specialized Surgical Procedures
Our laparoscopic surgeons also perform minimally invasive surgery for:
- Emergency surgical interventions
Revolutionary Benefits of Minimally Invasive Surgery
1. Dramatically Reduced Scarring
Traditional open surgery often results in large, visible scars that can affect patient confidence and comfort. Minimally invasive surgery creates tiny incisions that heal with minimal scarring, providing superior cosmetic outcomes that patients appreciate long after their recovery.
2. Accelerated Recovery Times
One of the most significant advantages of minimally invasive treatments is the dramatically reduced recovery period. Since laparoscopic surgery causes less tissue trauma, patients experience:
- Faster return to normal activities
- Reduced time away from work and family responsibilities
- Earlier resumption of exercise and physical activities
- Same-day discharge for many procedures
3. Significant Pain Reduction
Minimally invasive surgery substantially reduces postoperative pain compared to traditional open procedures. This benefit translates to:
- Decreased reliance on strong pain medications
- Reduced risk of medication-related side effects
- Improved patient comfort during recovery
- Better overall surgical experience
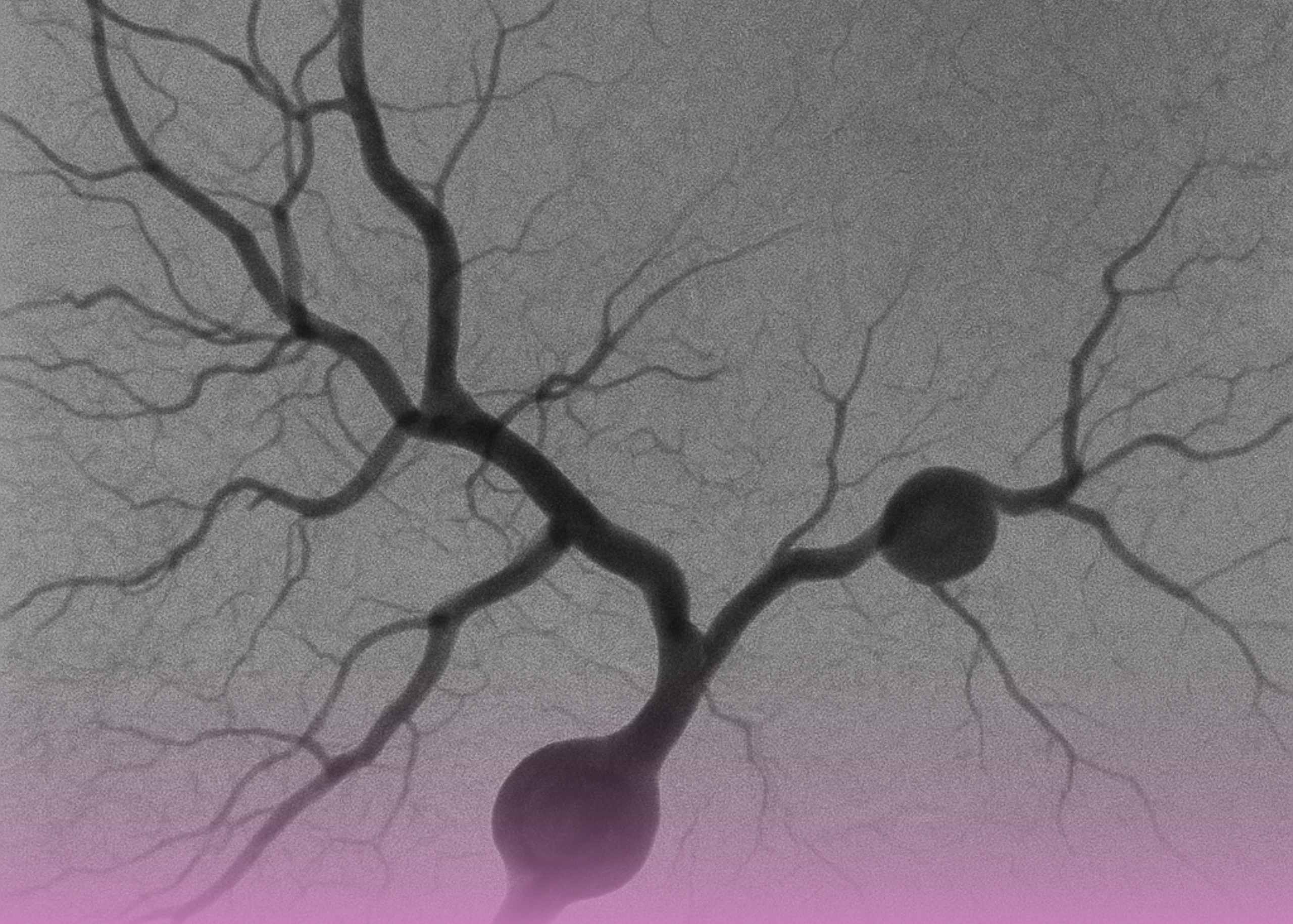
4. Lower Complication Rates
Laparoscopic surgery performed by experienced general and laparoscopic surgeons offers enhanced safety profiles:
- Reduced Infection Risk: Smaller incisions minimize bacterial exposure and contamination
- Decreased Bleeding: Precise surgical techniques result in minimal blood loss
- Lower Risk of Adhesions: Less tissue manipulation reduces the formation of internal scar tissue
- Reduced Anesthesia Requirements: Shorter procedure times mean less exposure to anesthesia
5. Enhanced Surgical Precision
Modern minimally invasive surgery provides laparoscopic surgeons with superior visualization and control:
- High-definition imaging reveals anatomical details impossible to see with traditional methods
- Magnification capabilities allow for identification of minute structures
- Steady, tremor-free instrument control improves surgical accuracy
- Better preservation of healthy tissues surrounding the surgical site
6. Shorter Hospital Stays
Minimally invasive treatments often allow patients to return home the same day or within 24 hours of surgery. This benefit provides:
- Lower risk of hospital-acquired infections
- Increased patient satisfaction
- Faster return to familiar surroundings
Advanced Technology in Minimally Invasive Surgery
State-of-the-Art Equipment
Burjeel Medical City invests in the latest minimally invasive surgery technology to ensure optimal patient outcomes:
- High-Definition Imaging Systems: Crystal-clear visualization for enhanced surgical precision
- Advanced Insufflation Systems: Controlled gas introduction for optimal surgical workspace
- Specialized Instruments: Purpose-built tools designed specifically for laparoscopic surgery
- Robotic Surgical Platforms: Cutting-edge technology that enhances traditional laparoscopic surgery capabilities
Integration of Artificial Intelligence
Our minimally invasive treatments benefit from AI integration that assists laparoscopic surgeons in:
- Real-time decision-making during procedures
- Enhanced imaging interpretation
- Predictive analysis for optimal surgical planning
- Continuous improvement in surgical techniques
Choosing the Right Minimally Invasive Treatment
Patient Evaluation Process
Determining candidacy for minimally invasive surgery involves comprehensive evaluation by our expert laparoscopic surgeons:
Medical History Assessment: Complete review of patient’s health status, previous surgeries, and current medications
Physical Examination: Thorough evaluation to determine the most appropriate surgical approach
Diagnostic Testing: Advanced imaging and laboratory studies to guide treatment planning
Risk-Benefit Analysis: Careful consideration of individual patient factors and surgical options
Factors Influencing Treatment Selection
Our laparoscopic surgeons consider multiple factors when recommending minimally invasive treatments:
- Condition Severity: Complexity and extent of the medical condition
- Patient Health Status: Overall fitness and ability to tolerate surgery
- Previous Surgical History: Impact of prior procedures on current treatment options
- Patient Preferences: Individual goals and expectations for surgical outcomes
Expertise You Can Trust: Our Laparoscopic Surgeons
Board-Certified Specialists
Burjeel Medical City’s laparoscopic surgeons represent the pinnacle of surgical expertise:
- Advanced Training: Specialized fellowship training in minimally invasive surgery techniques
- Extensive Experience: Thousands of successful laparoscopic surgery procedures
- Continuous Education: Ongoing participation in the latest minimally invasive surgery developments
- Research Contributions: Active involvement in advancing minimally invasive treatments
Multidisciplinary Approach
Our minimally invasive surgery program involves collaboration between:
- Expert laparoscopic surgeons
- Specialized anesthesiologists
- Advanced imaging specialists
- Postoperative care coordinators
Recovery and Follow-Up Care
Immediate Postoperative Period
Following minimally invasive surgery, patients experience:
- Minimal postoperative discomfort
- Rapid mobilization and early ambulation
- Quick return of normal bodily functions
- Same-day or short-stay discharge in most cases
Long-Term Outcomes
Minimal invasive surgery performed by our expert laparoscopic surgeons provides:
- Excellent long-term results with minimal complications
- Preserved organ function and anatomical integrity
- High patient satisfaction rates
- Improved quality of life compared to traditional surgery
Comprehensive Follow-Up Program
Our commitment to minimally invasive treatments extends beyond the operating room:
- Regular postoperative appointments with laparoscopic surgeons
- Comprehensive monitoring of healing progress
- Prompt attention to any concerns or questions
- Long-term surveillance for optimal outcomes
The Future of Minimally Invasive Surgery
Emerging Technologies
Minimally invasive surgery continues to evolve with innovations such as:
- Single-Port Surgery: Further reduction in incision size and number
- Flexible Robotics: Enhanced maneuverability for complex anatomical spaces
- Augmented Reality: Real-time overlay of imaging data during laparoscopic surgery
- Artificial Intelligence Integration: Smart surgical assistance for improved outcomes
Expanding Applications
The scope of minimally invasive treatments continues to broaden, with new applications being developed for:
- Complex cardiac procedures
- Advanced oncological surgeries
- Pediatric surgical conditions
- Emergency surgical interventions
Why Choose Burjeel Medical City for Minimally Invasive Surgery?
Excellence in Patient Care
As a leading healthcare institution, Burjeel Medical City offers:
- World-class laparoscopic surgeons with international training and certification
- State-of-the-art surgical facilities equipped with the latest minimally invasive surgery technology
- Comprehensive minimally invasive treatments across multiple medical specialties
- Patient-centered care focused on optimal outcomes and satisfaction
Commitment to Innovation
Our dedication to advancing minimally invasive surgery includes:
- Continuous investment in cutting-edge technology
- Ongoing training and education for laparoscopic surgeons
- Research and development in minimally invasive treatments
- Collaboration with international medical centers and experts
Comprehensive Support Services
Beyond surgical expertise, patients benefit from:
- Thorough preoperative education and preparation
- Dedicated patient coordinators for seamless care
- Advanced pain management protocols
- Comprehensive discharge planning and follow-up care
Making the Right Choice for Your Health
Minimally invasive surgery represents the gold standard in modern surgical care, offering patients safer, more comfortable, and more effective treatment options. Our expert laparoscopic surgeons at Burjeel Medical City are committed to providing the highest quality minimally invasive treatments tailored to each patient’s unique needs.
Whether you require laparoscopic surgery for a common condition or advanced minimally invasive treatments for complex medical issues, our team combines technical expertise with compassionate care to ensure optimal outcomes.
Take the Next Step Toward Better Health
If you’re considering surgical treatment, explore the advantages of minimally invasive surgery with our best laparoscopic surgeons in Abu Dhabi . Contact Burjeel Medical City today to schedule a consultation and discover how minimally invasive treatments can provide the safe, effective, and comfortable surgical experience you deserve.
Experience the future of surgery today with minimally invasive surgery at Burjeel Medical City – where innovation meets compassionate care for optimal patient outcomes.
Our Experts