In a remarkable surgical achievement, specialists at Burjeel Hospital have successfully treated a rare vascular condition that affects only a tiny fraction of the population worldwide. The patient presented with debilitating symptoms that were successfully resolved through an innovative surgical approach.
Extremely Rare Diagnosis
A young male patient arrived at Burjeel Hospital with short-distance claudication – severe pain that occurred after walking only brief distances. This symptom significantly limited his mobility and quality of life, prompting a thorough diagnostic investigation.
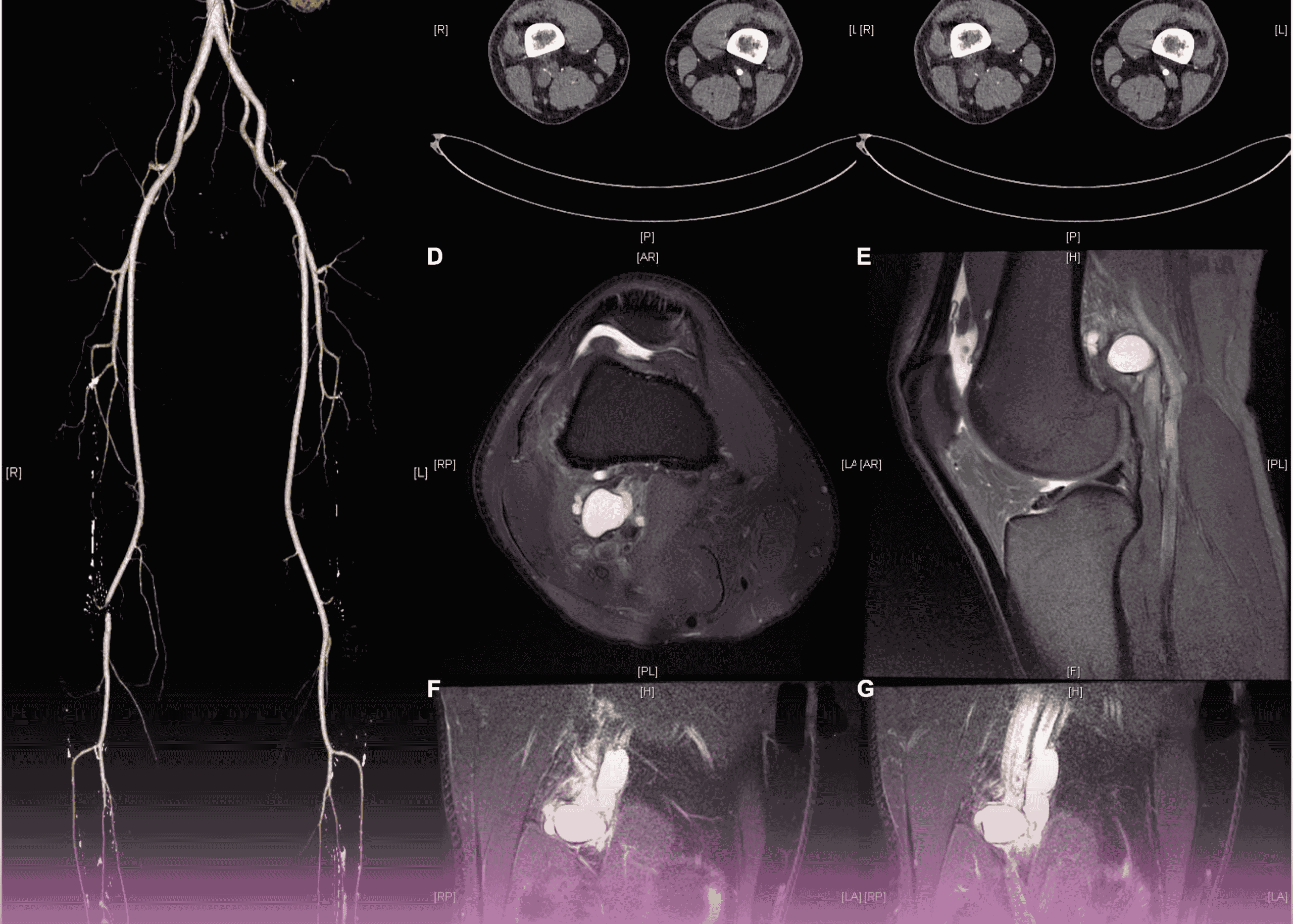
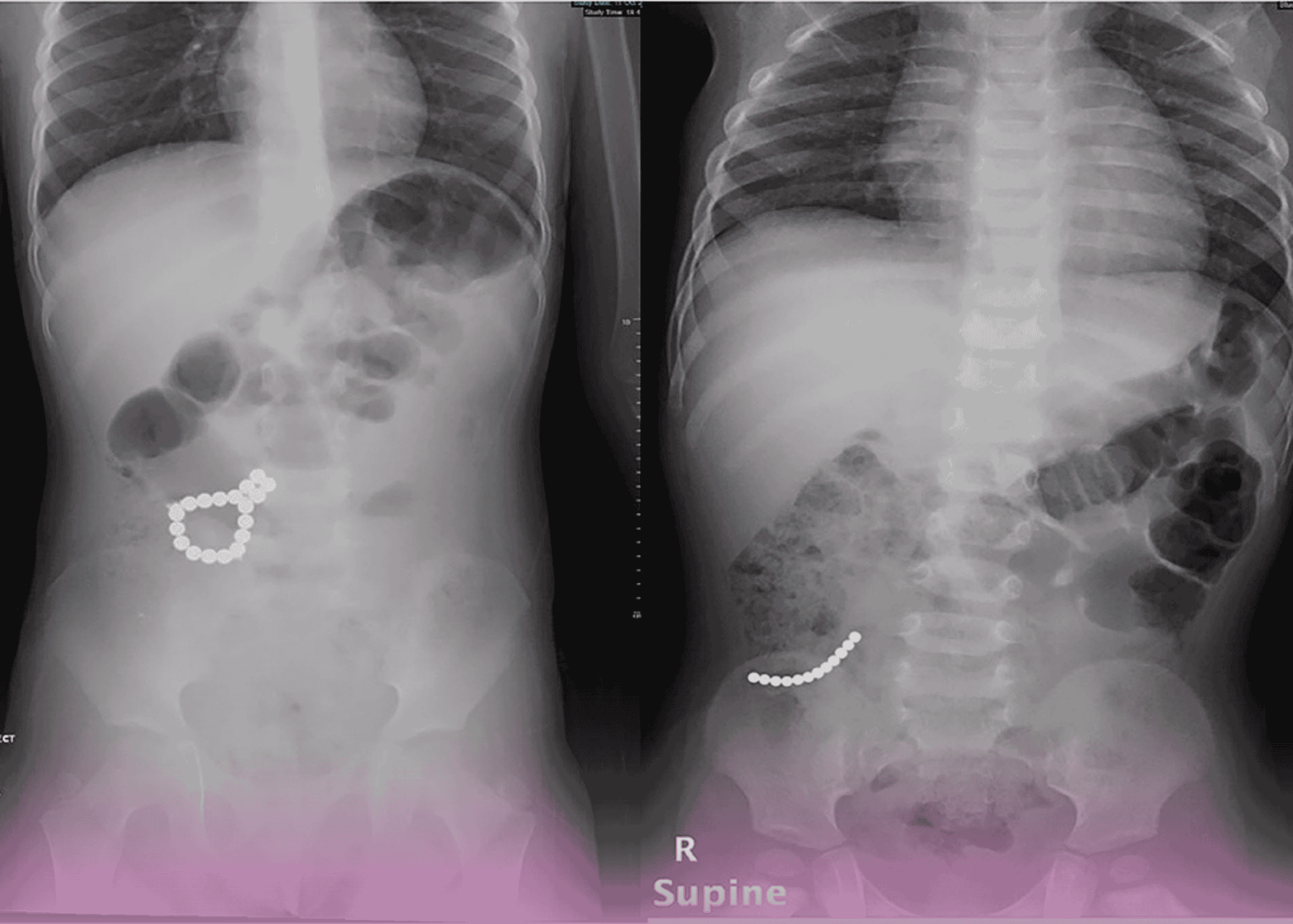
CT angiogram and MRI examinations of the right knee revealed an unusual finding: cystic adventitial disease affecting the popliteal artery. This exceedingly rare vascular disorder involves cystic degeneration in the wall of an artery, most commonly occurring in the popliteal artery behind the knee.
“Since its first description in 1947, only about 300 cases have been reported worldwide,” explains Dr. Moatasiem Bukhari, Consultant Vascular Surgeon at Burjeel Hospital. “This makes it one of the rarest vascular conditions we encounter in clinical practice.”
Tissue biopsy confirmed the diagnosis, and the case was thoroughly reviewed in Burjeel’s Vascular Multidisciplinary Team meeting, where specialists concurred on the optimal approach to treatment.
Surgical Management Challenges
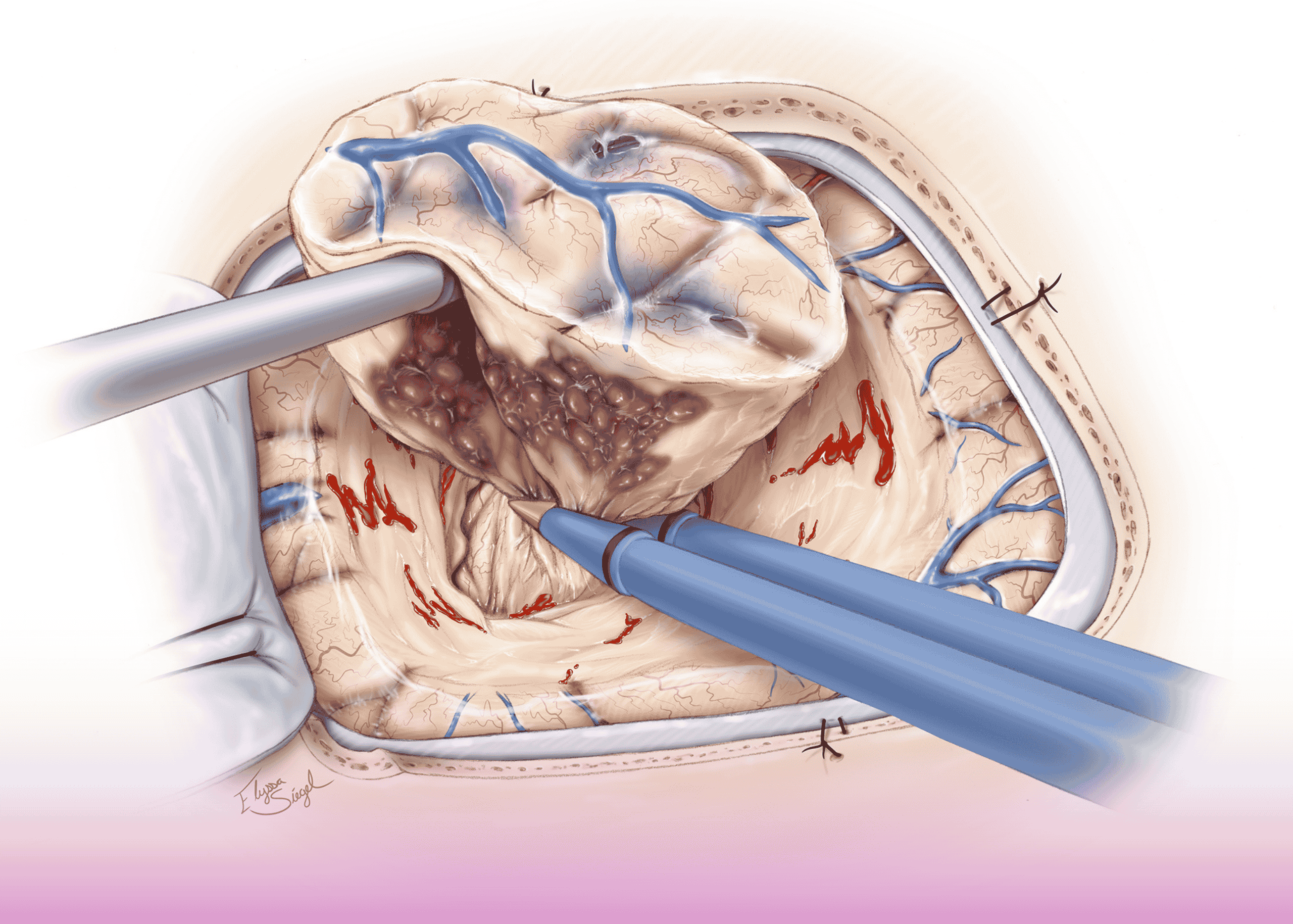
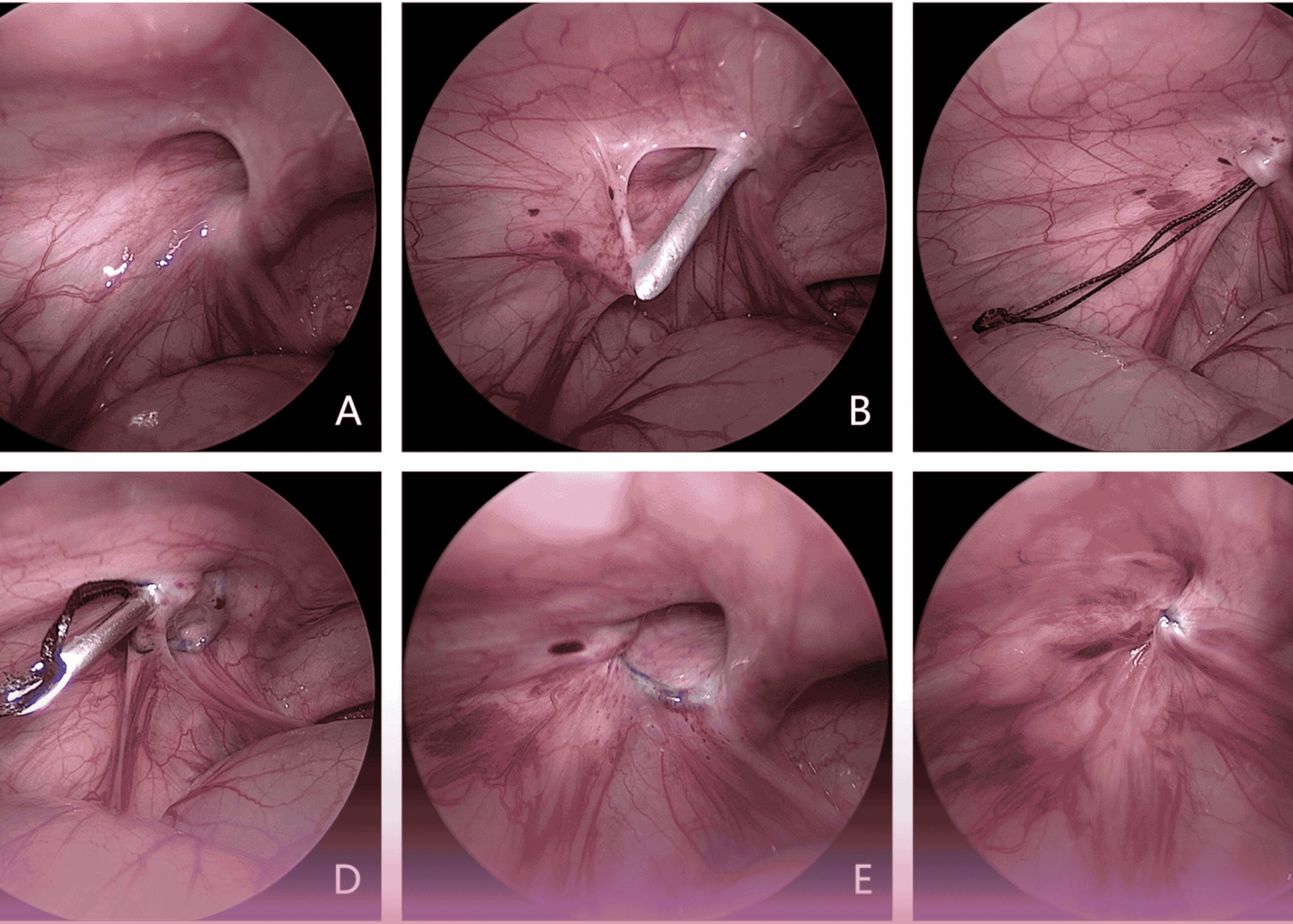
The consensus was to perform an open surgical procedure using a posterior approach to access the affected area. This challenging operation was further complicated by several factors:
- The rarity of the condition, with minimal precedent cases for reference
- Severe inflammatory changes affecting both the artery itself and surrounding tissues
- The compact anatomical space of the popliteal fossa where the affected artery was located
- This was the first such case to be treated within the Burjeel Holdings hospital network
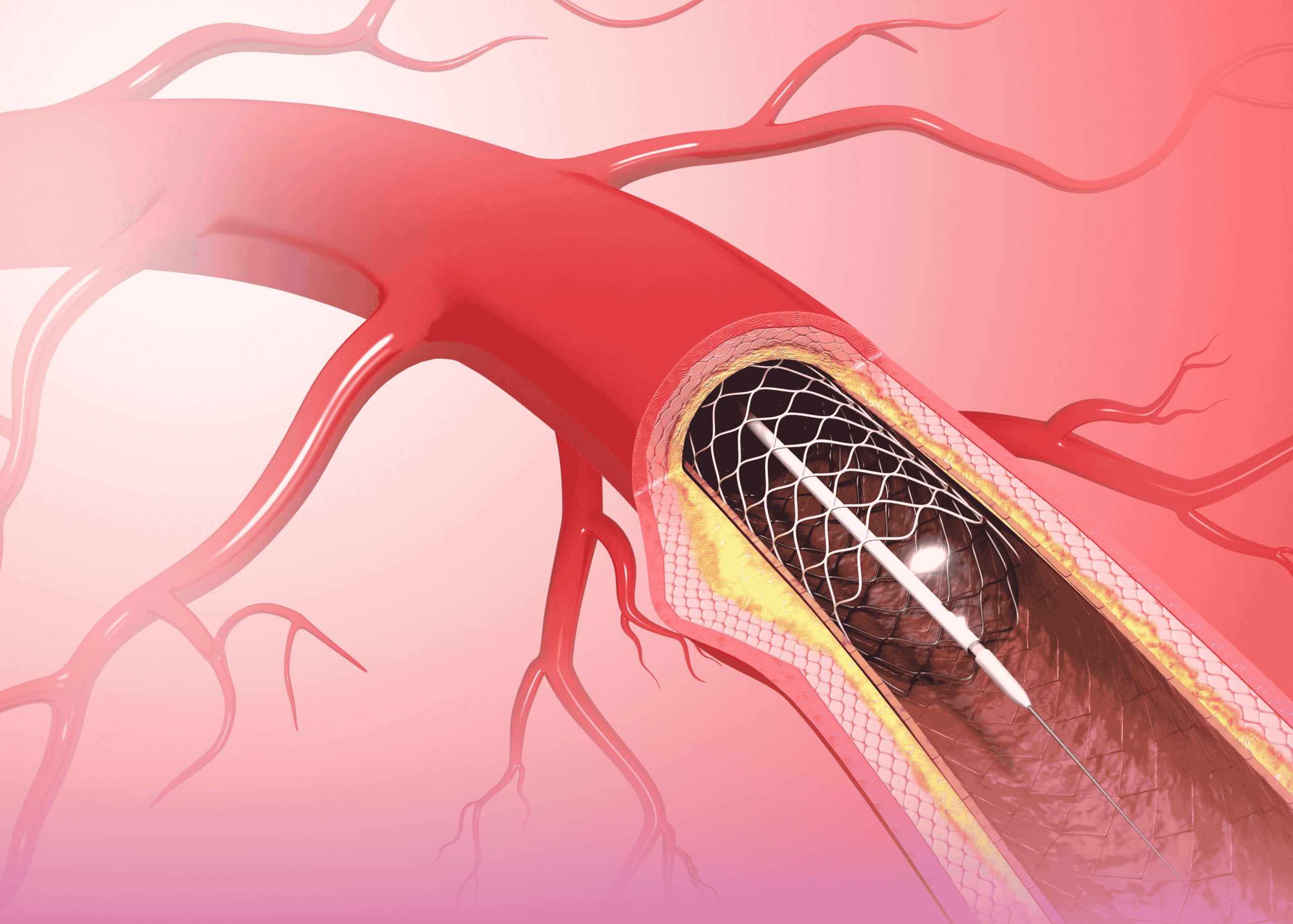
The surgical team successfully performed an interposition graft procedure, using the patient’s own long saphenous vein from the same leg to create a bypass around the affected arterial segment. This approach preserves blood flow while eliminating the diseased portion of the vessel.
Excellent Patient Outcome
Following surgery, the patient remained in the hospital for five days for observation and recovery before being discharged in good health. The procedure restored normal blood flow to the lower extremity, alleviating the painful claudication symptoms and allowing the patient to resume normal daily activities.
This case exemplifies the specialized expertise available at Burjeel Hospital for treating even the most uncommon vascular conditions. The successful outcome resulted from meticulous diagnosis, careful surgical planning, and the precise execution of a complex vascular procedure.
The case underscores the importance of considering rare vascular disorders in the differential diagnosis of patients with atypical claudication symptoms, particularly in younger individuals without traditional risk factors for peripheral arterial disease.