Patients suffering from complex regional pain syndrome (CRPS) often experience debilitating symptoms that significantly impact their quality of life. At Burjeel Day Surgery Center, specialists are employing advanced interventional pain management techniques to provide relief for these challenging cases.
Understanding Complex Regional Pain Syndrome
CRPS is a disabling condition that typically affects limbs following an injury or surgery. The condition manifests through severe pain, swelling, limited range of motion, temperature changes, and skin discoloration. While the definitive pathology remains incompletely understood, current evidence suggests CRPS involves immune system disruption affecting the nervous system.
Dr. Shailendra Chauhan, Consultant Anesthesia and Pain Management at Burjeel Day Surgery Center, explains: “CRPS is categorized into two types: Type 1 (Reflex Sympathetic Dystrophy) when there is no obvious nerve injury, and Type 2 (Causalgia) when there is a clear nerve injury. Both types present with overlapping symptoms but differ in their underlying mechanisms.”
Diagnosis relies on clinical criteria such as the Budapest Criteria, which evaluates sensory, vasomotor, sudomotor/edema, and motor/trophic changes to establish the presence of CRPS.
Targeted Intervention
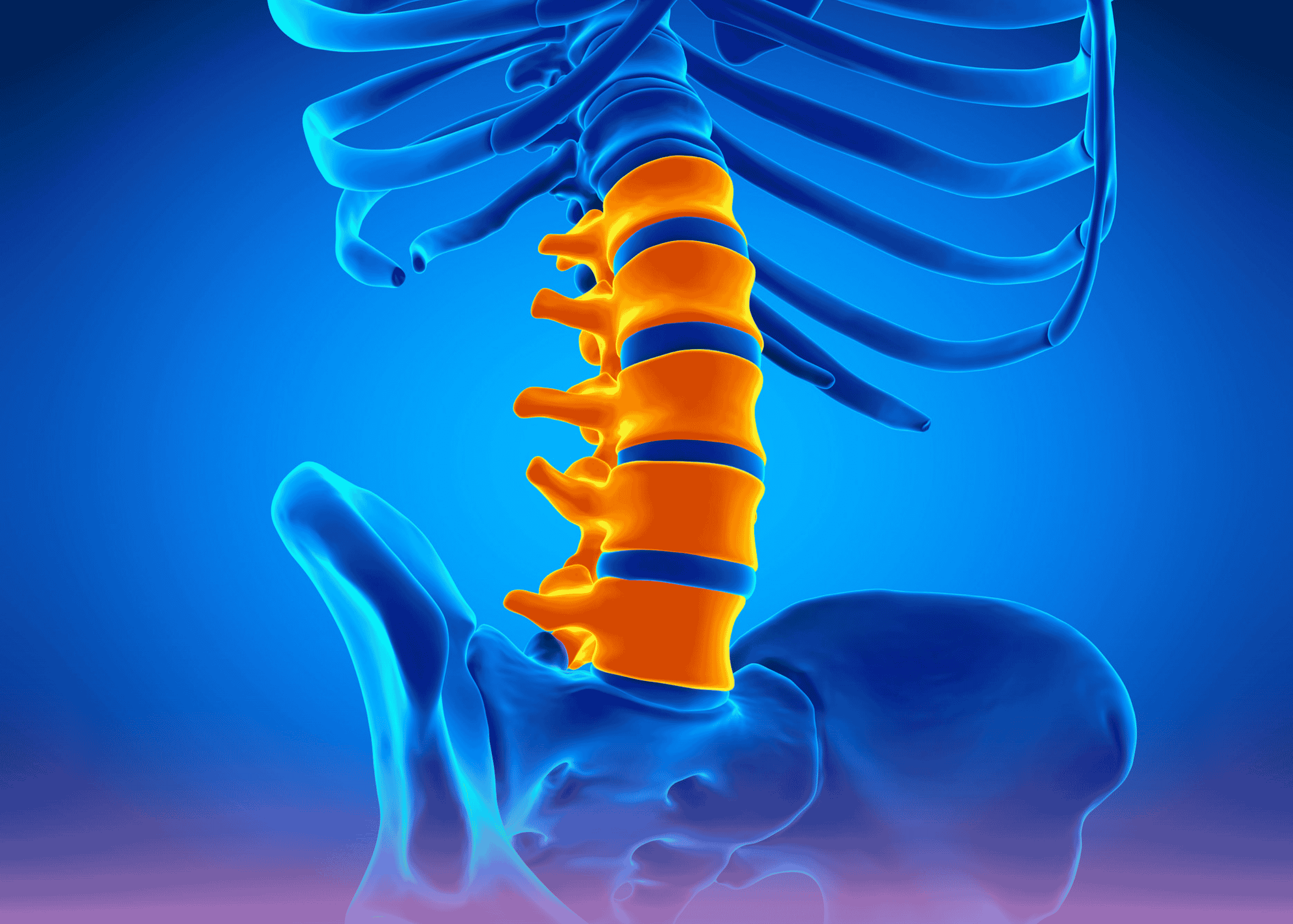
A lumbar sympathetic block is a minimally invasive pain procedure designed to disrupt nerve signals from the sympathetic chain to the lower extremities. This intervention is particularly valuable for various painful conditions, including CRPS, phantom limb pain, hyperhidrosis, vascular insufficiencies, and herpes zoster.
“The densest portion of the lumbar sympathetic ganglia is located at the L2 and L3 vertebral levels,” notes Dr. Chauhan. “For optimal results, we typically perform the initial diagnostic block at the L3 level using only local anesthetic. If significant relief is achieved, we proceed with radiofrequency ablation at L2, L3, and L4 levels for longer-lasting benefit.”
Case Study: Post-Surgical CRPS
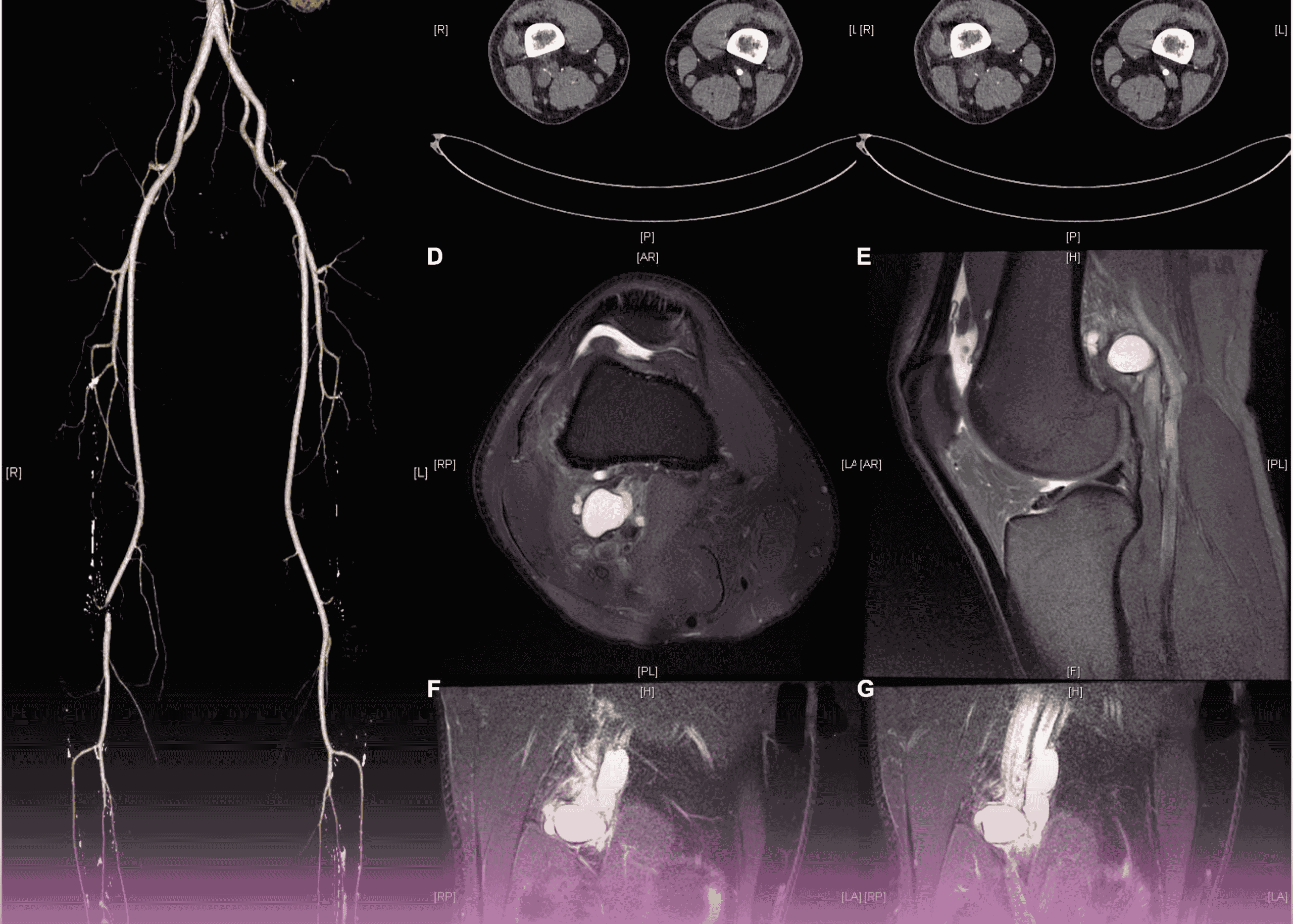
A young male patient was referred from the orthopedic department after developing CRPS following right knee surgery three months prior. His presentation included:
- Elevated skin temperature around the knee
- Moderate to severe pain (VAS 7/10)
- Mild swelling
- Hypoesthesia (decreased sensation) along the lateral aspect of the limb
- Allodynia (pain from normally non-painful stimuli) along the anterior aspect
Conservative management had failed to provide adequate relief, prompting consideration of interventional techniques.
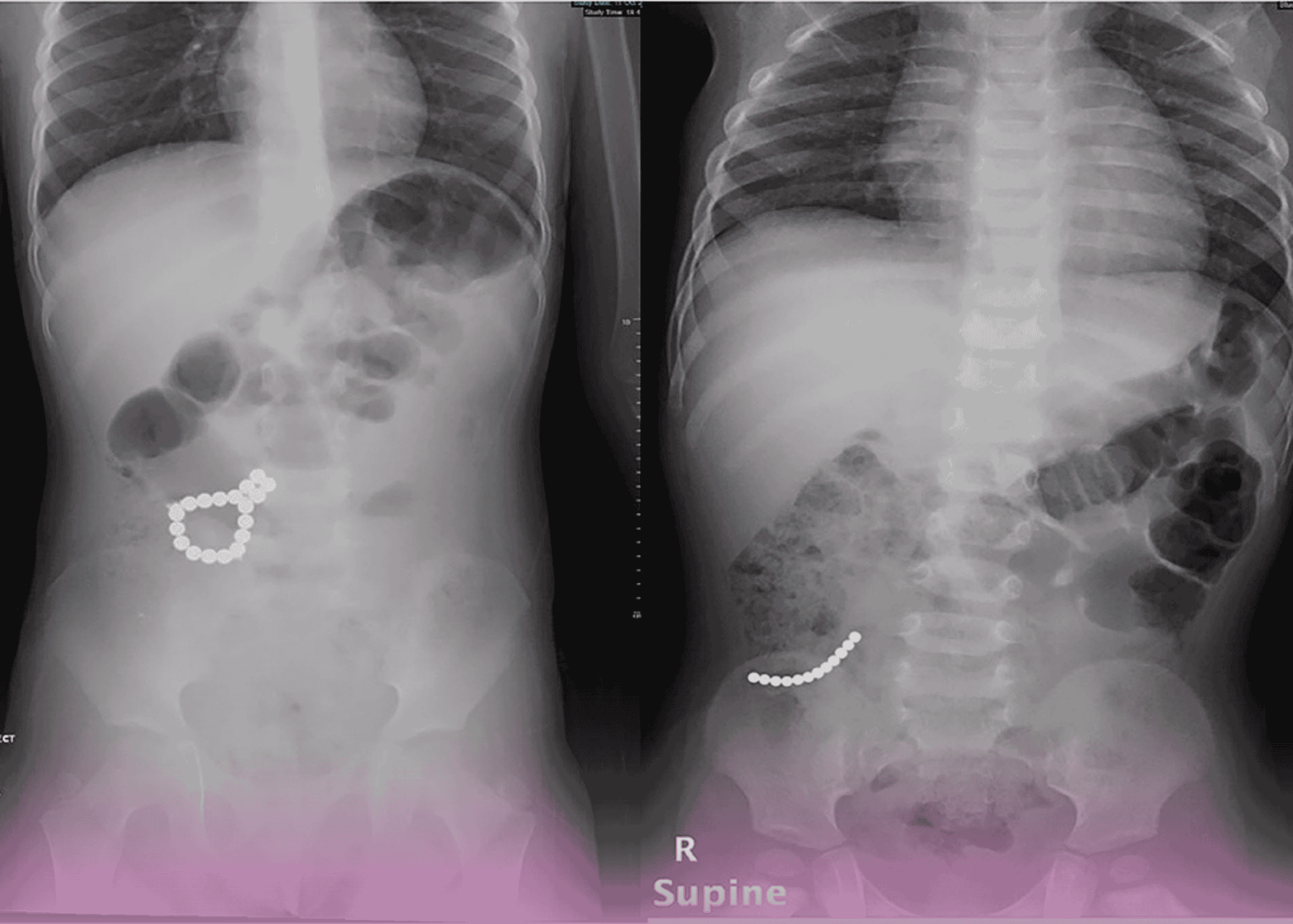
After thorough counseling and informed consent, the patient underwent a lumbar sympathetic diagnostic block at the right L3 level. The procedure was performed under fluoroscopic guidance to ensure precise needle placement.
Remarkable Results
Following the diagnostic block, the patient experienced immediate pain relief and demonstrated improved range of motion in the affected knee. This dramatic response confirmed the sympathetic nervous system’s involvement in his pain condition and established him as an excellent candidate for radiofrequency ablation.
The patient was subsequently scheduled for radiofrequency ablation, which involves creating controlled lesions to interrupt pain signals for a longer duration than temporary nerve blocks allow. This comprehensive treatment plan will continue at Burjeel Day Surgery Center, Al Reem.
“While CRPS typically doesn’t have a definitive cure, timely interventions like lumbar sympathetic blocks can significantly slow disease progression and provide crucial pain relief, helping patients maintain daily function and quality of life,” Dr. Chauhan emphasizes.
This case highlights the importance of a multidisciplinary approach to chronic pain conditions and the value of specialized interventional techniques in managing complex pain syndromes refractory to conventional medical management.