There are several tips and tricks to eating healthy. Many of these ideas can be challenging to accomplish in today’s busy world. Still, they can give you the edge you’ve been looking for in a healthy lifestyle.
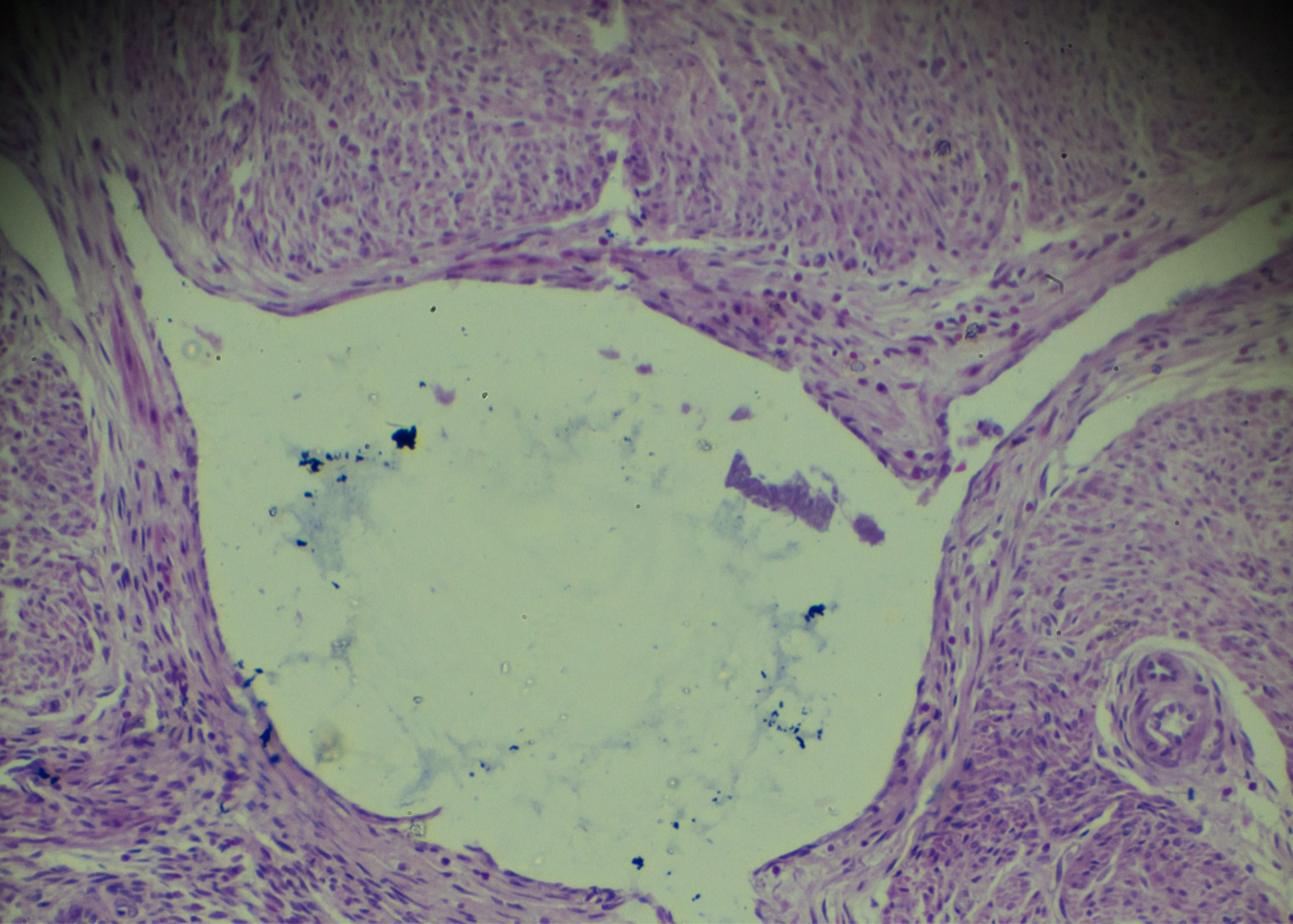
How Does a Healthy Plate Look Like?
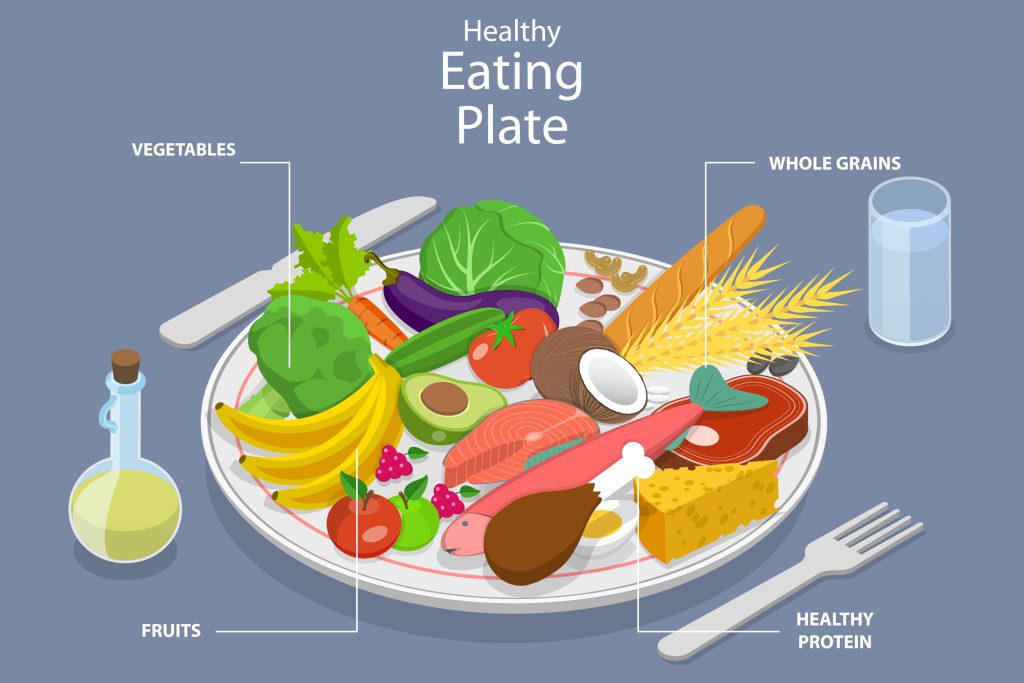
- ¼ of the plate with grains, choose at least 50% whole grains (whole wheat bread, Brown Rice, etc.).
- ¼ of the plate with protein choices vegetarian or non-vegetarian, choose eggs, fish, lean meat, chicken, beans, cheese, and nuts.
- ½ of the vessel to be loaded with colorful fruits and veggies.
- Hydrate adequate. Drink water- 30ml/kg body weight is the requirement. Find yours and start to sip.
Fruit vs Fruit Juice

Fruit
- 62 Kcal
- More Fiber
- Less concentrated fructose
- Fewer calories
- Lower glycemic index
Juice
- 112 Kcal
- Less fiber
- More concentrated fructose
- More calories
- Higher glycemic index
How to Include Fruits in the Diet

- Snack on fruits
- Try fruit as dessert
- Delight your sweet tooth by eating healthy with fresh fruit yogurt, parfaits, and dried fruits
- Including fruit with breakfast or as dinner snacks is eating healthy
What is One Serving of Fruit?

- 1 medium-size fruit
- ½ cup fruit salad
- ¼ cup Dried fruits
- ½ cup fresh juice
- Include at least two servings of fruit a day
Are You Drinking Enough Water?

How Much Water Should You Drink Per Day?
30 ml X Actual body weight (Kg) Note: Restrict fluids; if any medical conditions, or if recommended by the Physician
- Thirst is the first signal of Dehydration
- Check the urine color
- The dark color indicates dehydration
- Lighter the color, better hydration
- Dry skin
- Dry lips
- Less urination
- Feeling tired, dizzy, and headaches
How to increase water intake?
- Keep a water bottle next to you or a reachable place.
- Use a mobile app to remind and measure your intake.
- Fancy bottles attract and improve the intake.
- Infused water (Lemon, Ginger, and Mint) to enhance the taste.
What is the Healthy Thing to Snack on?

Most times the snacks are the unhealthiest stuff chosen. Portion-sized healthy snacks are a great way to follow small frequent meal patterns.
A healthy snack
- Being between meal times is a good option to decrease hunger and prevent overeating at meal times.
- boosts the metabolism, sustains the energy levels, and can overcome cravings.
- to be chosen wisely, because unhealthy snacks lead to weight gain.
- should be low in sugar, salt, and fat.
- can be fruit or veggie salad or whole-grain snacks or low-fat dairy instead of junk.
- can be a combination of Protein + Carbohydrate choices that can keep the stomach full for a longer time. Eg: Yogurt and fruits, Hummus with Vegetable sticks or cheese with fruit slices, etc.
Some sensible snack replacements:
- Mixed nuts( 1 ounce)
- Low-fat Yogurt/ laban (1 cup)
- Fruits (1 serving)
- Dark Chocolate (30 gm)
- Air Popped Popcorn( 3 cups)
Why Is Fiber Good for You?

Benefits:
- Helps maintain bowel health and Prevents constipation.
- Helps in lowering blood cholesterol levels.
- Helps in better control of blood sugar levels.
- Keeps the stomach full.
- Aids achieving healthy body weight.
Recommendation:
- 14g of fiber for every 1000Kcal
- Females: 25g/day Males: 38g /day
Tips to increase fiber in your diet
- Include lean veg proteins-Beans, peas, and lentils.
- Snack on nuts and seeds.
- Increase your fruit and vegetable intake.
- Have the fruit instead of the juice.
- Don’t peel the fruit or veg before consuming it.
- Go for whole-grain products (at least 50% can be whole grains).
How Physically Active Are You?

Inactive: less than 5,000 steps per day
Average (somewhat active): ranges from 7,500 to 9,999 steps per day
Active: more than 10,000 steps
Very active: more than 12,500 steps per day
Tips to Include More Steps to Your Day

- Park farther away
- Walk while waiting
- Take the stairs
- Consider a walk with the family
- Take your pet for a walk
- Take the farthest way
- Talk in person. Rather than instant-messaging or emailing with coworkers, get up and walk to their desks
- Walk during your kids’ activities
- Start increasing your goal gradually by adding 500-1000 extra steps every 3-4 days
Health Benefits of Being Physically Active:

It reduces your risk of:
- Heart diseases
- Obesity
- Diabetes
- Depression
- Elevated blood pressure
- Elevated cholesterol levels
You are What You Eat

Plan Balanced Diet
- Eating healthy means planning ahead and trying to include all the possible 5 groups in each meal- fiber-rich grains, lean protein choices, fruits, vegetables, and low-fat dairy products.
Adopt Healthy Cooking
- Try to avoid deep-fried foods. Choose healthy cooking methods like baking, broiling, steaming, grilling, or roasting.
Utilize Time Efficiently to Plan
- Chop fresh vegetables and fruits and store ahead for quick preparation.
- Prepare the grocery list based on the requirement.
Flavor the Food
- Use herbs, spices, low salt seasonings, or lemon juice to cook vegetables and meat.
- Cut down the use of salt as much as possible.
Curb the Sweet Tooth
- Include berries, dried fruits, and dark chocolate, and prepare healthy and quick desserts like yogurt parfait, granola parfaits, smoothies, chia seed pudding, etc instead of sugar-loaded stuff.
Learn to Read Nutrition Labels and Choose Wisely
- Check for salt, sugar, and fat content of the packed foods. Look for the serving sizes to understand the portion sizes.
How to Improve Your Hair Health?

Nutritional deficiency may impact both hair structure and hair growth. Effects on hair growth include the result of sudden weight loss or decreased protein intake, niacin deficiency, or any underlying medical condition.
- Eating healthy, and balanced diet with a lot of antioxidants might help prevent nutritional deficiencies.
- Some major nutrients that benefit and add to our hair health are Vitamin A, C, Vitamin D, Vitamin E, Biotin, Iron, Zinc, Selenium, Proteins, and Omega 3 fatty acids.
- Consuming foods rich in the above nutrients is beneficial, Eg: Citrus fruits, Oily fish, nuts and seeds, eggs, sweet potato, avocado, pumpkin, chia seeds, yogurt, spinach, asparagus, chickpeas, etc.
- Avoid excess consumption of processed food that leads to your body getting deprived of nutrients.
- Managing stress and developing good sleep patterns are add-on benefits.
- Don’t depend on supplements without consulting the physician. Overdose of these supplements might be toxic.
Mind Your Salt

Salt is an important seasoning, flavoring agent, and preservative. Sodium in salt is one of the essential minerals and performs vital functions in the body. A diet high in salt (or sodium) can raise blood pressure, which can increase your risk of heart disease and stroke.
Tips to limit your sodium/salt intake
- Avoid processed foods and buy fresh foods.
- Rinse the sodium-containing canned foods.
- When dining out, ask restaurants to limit the salt.
- Portion control while eating out.
- Cook your food whenever possible to avoid instant noodles/ soups/frozen meals.
- Substitute the salt with spices, lemon, garlic, and herbs to flavor your food. This practice can make your eating healthy.
- Always read the food label.
- Try to have salt free/ low-salt snacks.
Reading the labels on your food package
- Salt/sodium-free – less than 5mg of sodium per serving.
- Very low sodium – 35mg of sodium or less per serving.
- Low sodium – 140mg of sodium or less per serving.
- Reduced sodium – at least 25% less sodium than the regular product.
- Lightly salted – at least 50% less sodium than the regular product.
Eat Fat to Lose Fat

A small amount of fat is an essential and important part of eating healthy diet. The dietary reference intake for fats in adults is 20% to 35% of total calories per day. Fat is the source of essential fatty acids that our body cannot produce. It is important to include healthy fats in the diet.
Make sure you get most of your fat intake from unsaturated fat options. Unsaturated fats are found in plant foods and oily fish, and they are usually liquid at room temperature. They’re found in:
- Oils from vegetables, nuts, and seeds, such as sunflower, safflower, olive, walnut, and corn oil
- Spreads based on these oils
- Nuts and seeds
- Avocado
- Oily fish such as herring, sardines, mackerel, salmon, and trout
Benefits of unsaturated fats:
- Lower the risk of heart disease and stroke.
- Lower bad LDL cholesterol levels, while increasing good HDL.
- Support anti-Inflammatory Process
- Essential for the absorption of A, D, E, and K vitamins
- Optimize nerve and brain function
- Improves and softens your skin
Keep Your Skin Radiant & Healthy

- Water is “the forgotten nutrient”. It gets rids the body of harmful toxins that can clog the pores. Drink at least eight glasses of water a day.
- Vitamin C keeps the skin look plump and wrinkle-free. Include citrus fruits, red peppers, and dark green leafy greens like kale, strawberries, and kiwis.
- An inflamed gut means inflamed skin. Include probiotics regularly in the diet to heal the gut. Try sauerkraut, anything pickled, yogurt with live active cultures, kefir, and miso.
- Prebiotics in the diet help to feed the healthy flora and restore the gut microbiome to a much more healthy state. Include Garlic, leeks, and asparagus—those are great sources of prebiotic fiber in the diet
- Antioxidants protect against free-radical damage—doing wonders for the skin! Include Berries (Blueberries, blackberries, cranberries and goji berries, kale, beets, and spinach).
Is Coffee Bad for You?

World Health Organization (WHO) has taken coffee off the possible carcinogen list. And there’s increasing evidence that coffee might actually be good for you. Studies have found that coffee drinkers may have a reduced risk of:
- Cardiovascular disease (including heart attack, heart failure, and stroke)
- Type 2 diabetes
- Alzheimer’s disease and Parkinson’s disease
- Colon, uterine, and liver cancer
- Cirrhosis
- Avoid coffee if you have any health problems that require you to cut on caffeine
- Don’t have coffee on an empty stomach
- If you are a coffee drinker, make sure not to overconsume it, have it in moderation no more than 3-5 cups per day or on average 400mg of caffeine per day
- Make sure to avoid the extra calories, sugar, and saturated fat in coffee that is loaded with whipped cream or flavored syrups
- It is not necessary to drink coffee if you usually don’t as there are many other dietary strategies to improve your health