Thyroid disorders are a group of conditions that affect the thyroid gland. Thyroid disorders can cause a wide range of symptoms and can affect children, adults, and seniors. They also may be temporary or permanent, depending on your disease type.
What Does the Thyroid Gland Do?
The thyroid gland is a butterfly-shaped organ in the neck that produces hormones that help regulate metabolism. It’s located just below Adam’s apple and above the collarbone. It consists of two lobes, each with its thyroid tissue. A part of the brain controls the thyroid called the pituitary gland, which sends out hormones that tell your thyroid to make more or less of certain protein-based hormones. The thyroid can be affected by infections, physical injury, or radiation exposure. If it becomes overactive (hyperthyroidism) or underactive (hypothyroidism), it can cause problems with metabolism and lead to other health issues.
What is the Function of Thyroid Hormone?
Thyroid hormones are essential for the body’s proper growth, development, and function. They influence nearly every cell in the body, affecting growth, metabolism, and other complex processes. A feedback mechanism controls the production of thyroid hormones. The pituitary gland secretes a hormone called thyrotropin (TSH).
TSH signals the thyroid gland to produce more thyroid hormone when levels fall too low or less when they are too high. The thyroid gland produces two types of thyroid hormone: triiodothyronine (T3) and thyroxine (T4). T3 is the active form of the hormone; it stimulates cellular activity in almost every organ system in the body. In contrast, T4 is inactive until it is converted into T3 in target tissues such as muscle, bone marrow, and fat cells.
What are the Symptoms of Thyroid Hormone?
Signs and symptoms of a thyroid problem can include weight gain, especially around the midsection.
- Fatigue or lack of energy
- Muscle weakness or cramps
- Hair loss or thinning hair
- Cold intolerance (feeling cold even when others are warm) and unexplained chills
- Constipation or diarrhea, especially after eating, sometimes alternating between constipation and diarrhea.
- Dry skin that may feel coarse to the touch
What are the Causes of Thyroid Disorders?
Thyroid disorders are caused by the thyroid gland not producing enough hormones or by an overactive thyroid gland. The most common causes include the following:
- Iodine deficiency
- Autoimmune thyroid diseases
- Radiation exposure
- Congenital hypothyroidism
What are the Types of Thyroid Disorders?
Graves’ Disease
Graves’ disease is a condition that causes hyperthyroidism or an overactive thyroid gland. The thyroid gland is in the front of your neck, beneath your Adam’s apple. When someone has Graves’ disease, the immune system mistakenly produces antibodies that attack the thyroid gland and cause it to produce too much thyroid hormone. This can lead to several symptoms, including:
- Feeling overly energetic
- Weight loss despite increased appetite
- Hoarse voice (due to swelling in the throat)
- Increased sweating
- Irregular heartbeat (palpitations)
Hyperthyroidism
Hyperthyroidism is when the thyroid gland produces too much of the hormone thyroxine. The main treatment for hyperthyroidism is a medication that suppresses the production of thyroxine by the thyroid gland. Surgery may also remove part or all of the thyroid gland if the medication does not work well enough to control symptoms. The symptoms may include:
- Weight loss
- Heat intolerance
- Increased appetite
Hypothyroidism
Hypothyroidism is an underactive thyroid gland, which means the thyroid doesn’t produce enough hormones. It’s a condition that occurs when the body fails to secrete enough thyroid hormones. The symptoms of hypothyroidism include:
- Fatigue
- Weakness
- Constipation
- Dry skin and hair
- Weight gain and depression
Thyroid Cancer
Thyroid cancer is when abnormal cells form in the thyroid gland. The cause of thyroid cancer is not known. However, risk factors include exposure to radiation and certain chemicals, a family history of thyroid cancer, and being female and over 60 years old. Symptoms of thyroid cancer may include:
- A lump or swelling in your neck
- A sore throat that doesn’t go away with antibiotics
- Painless swelling in your neck or underarm
- Difficulty swallowing or breathing
- A cough or hoarseness that doesn’t go away
Thyroid Nodules
Thyroid nodules are small lumps that develop on the thyroid gland. Thyroid nodules are common and can develop due to an enlarged thyroid gland (goiter), inflammation, or irritation, or they may be caused by other conditions that affect your thyroid. If you have a thyroid nodule, it’s important to see your doctor for an evaluation to determine whether it is cancerous. The symptoms include:
- Difficulty swallowing
- Enlarged neck (goiter)
- Hoarseness or voice changes
- Difficulty breathing
- Pain in your neck or throat that feels like pressure or pain when you swallow
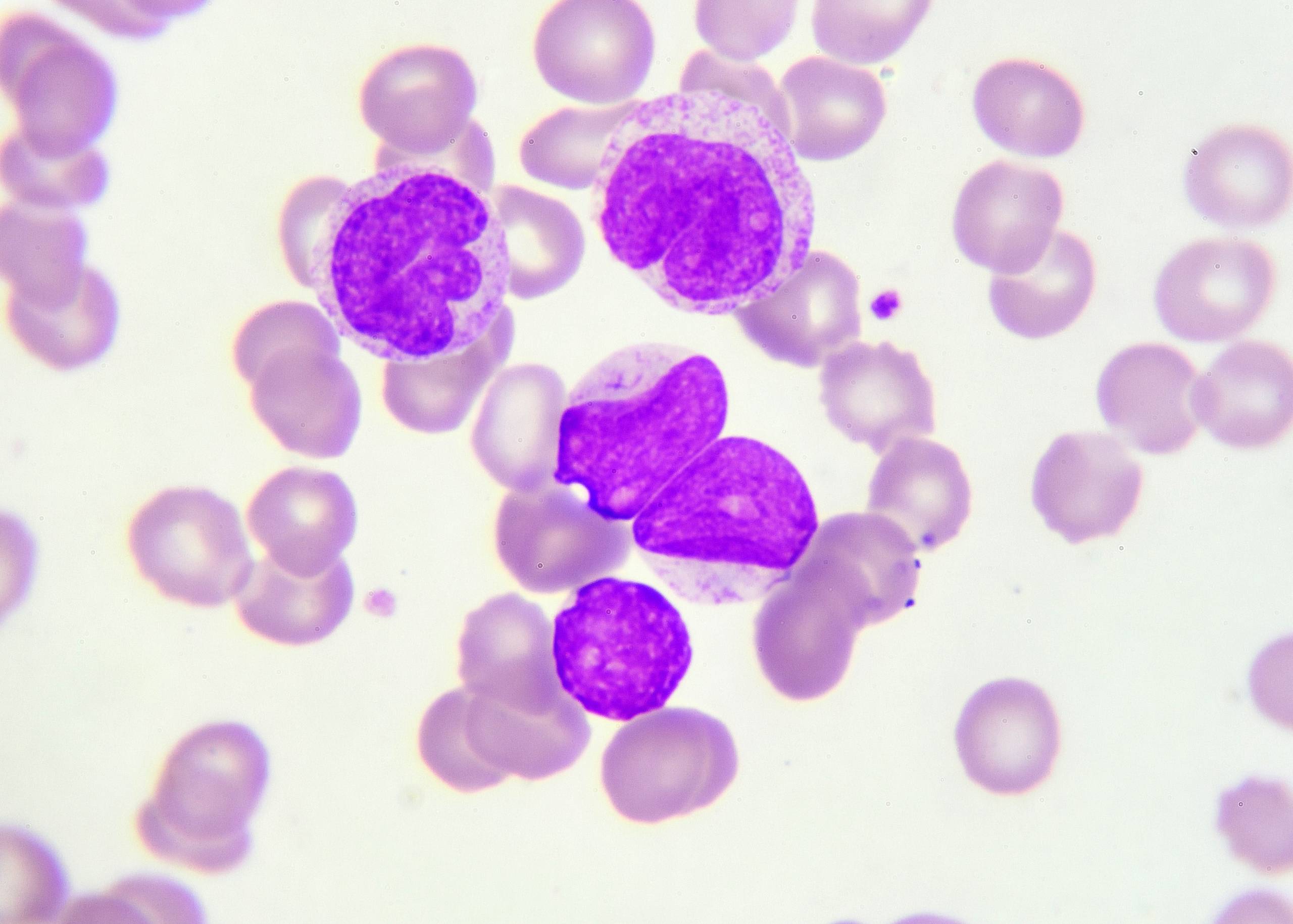
Hashimoto Thyroiditis
Hashimoto thyroiditis is when the immune system attacks the thyroid gland, causing thyroid inflammation. Hashimoto thyroiditis occurs when antibodies attack the cells in the thyroid gland, causing it to become inflamed. The antibodies are produced by a type of white blood cell called a T-lymphocyte. The body normally produces these antibodies to protect itself against viruses and bacteria, but in people with Hashimoto’s disease, these antibodies mistakenly attack healthy tissue. Hashimoto’s disease often appears gradually over time, with symptoms including:
- A hoarse voice
- Weight gain or difficulty losing weight
- Fatigue Sensitivity to cold temperatures
Silent Lymphocytic Thyroiditis (SLT)
Silent Lymphocytic Thyroiditis (SLT) is an autoimmune disease that causes a gradual deterioration of the thyroid gland. It’s known colloquially as “silent” because it doesn’t present with any symptoms, and it’s only discovered when a doctor orders a blood test for another reason. SLT is most common in women aged 15-35 with no other health problems. It can also affect men, but at a lower rate than women. Symptoms include:
- Low-grade fever
- Weight gain/loss
- Fatigue
- Tenderness or pain in the neck
Goiter
Goiter is a condition that causes the thyroid gland to enlarge beyond its normal size. Goiter usually occurs when there’s an iodine deficiency in the diet or water supply. Other causes include:
- The thyroid gland not producing enough thyroid hormone
- Excess iodine in the diet
- Excessive consumption of foods high in goitrogens (e.g., soy, cabbage, broccoli)
The most common symptom of goiter is swelling in the neck. The patient may also experience Difficulty Swallowing, Shortness of breath, and heart palpitations.
How are Thyroid Disorders Diagnosed?
Physical Examination
The doctor will work with several tests and procedures to determine whether or not you have a thyroid disorder. They will also look at factors like your family history, symptoms, and age to make a diagnosis. A physical exam is often the first step in diagnosing a thyroid disorder. Your doctor will look at your neck for signs of nodules or swollen lymph nodes and examine your throat and mouth for any unusual lumps or bumps. They may also listen to your heart and lungs and check your temperature, blood pressure, and weight.
Blood Tests
Diagnosis can be made through a blood test measuring thyroid-stimulating hormone (TSH), which is released by the pituitary gland in response to low levels of thyroid hormones. If the TSH level is greater than 4 mIU/L but less than 10 mIU/L, you may have hypothyroidism, which means your body isn’t producing enough thyroid hormone. If your TSH level is greater than 10 mIU/L but less than 50 mIU/L, you may have hyperthyroidism or too much thyroid hormone. If your TSH level is greater than 50 mIU/L and you also have symptoms such as weight loss or heart palpitations, then you may have Grave’s disease (hyperthyroidism). Suppose the symptoms don’t match any of these conditions. In that case, your doctor may order lab tests for thyroid antibodies—TSH receptor antibody (TRAb), thyroglobulin antibody (TgAb), anti microsomal antibody (AMA), thyroperoxidase antibody (TPOAb), and thyroid antimycobacterial peptide antibody (MAB).
Imaging Studies
Imaging tests can look at the thyroid gland’s size and shape, while thyroid ultrasound uses sound waves to create an image of the gland. They may also order imaging studies such as magnetic resonance imaging (MRI), or computed tomography (CT) scans if they suspect there’s something wrong with your pituitary gland or hypothalamus—the areas of the brain that control hormone production.
How are Thyroid Disorders Treated?
The treatment for thyroid disorders depends on the type of disorder, its severity, and the patient’s age. In most cases, treatment for thyroid disorders will involve taking a combination of medications and lifestyle changes to help manage symptoms. Medications used to treat thyroid disorders include
- Levothyroxine – a synthetic T4 hormone that replaces what you don’t have enough of in your body; it’s often used to treat hypothyroidism.
- Liothyronine – synthetic T3 hormone that replaces what you don’t have enough in your body; it’s often used to treat hypothyroidism.
- Thyroid hormone replacement therapy (THRT) replaces T3 and T4 hormones; this is often used when someone has had their thyroid removed surgically or accidentally damaged by radiation treatment.
- Antithyroid drugs – block the production or actions of thyroid hormones; they are prescribed as a last resort when hyperthyroidism is severe or uncontrolled by other treatments.
Thyroid Surgery
A thyroidectomy is a surgical procedure to remove the thyroid gland. Thyroidectomy is one of the most common surgeries performed on adults, and it’s often used to treat benign (non-cancerous) tumors and nodules in the thyroid gland. During a thyroidectomy, your doctor will remove all or part of your thyroid gland. Your surgeon may also remove lymph nodes from around your neck and any enlarged lymph nodes found near your vocal cords during surgery. This procedure can be done through a traditional “open” approach or a minimally invasive technique called robotic-assisted surgery (RAS), which uses computer-controlled surgical tools instead of traditional metal instruments. After surgery, you’ll stay overnight at the hospital for observation and then go home when you’re ready to resume normal activities. Most people can return to work within two weeks after having this surgery—but it depends on how many lymph nodes were removed during surgery and how quickly your body heals afterward.
At Burjeel Hospital in the United Arab Emirates, our endocrinologists are experts in diagnosing and treating all thyroid diseases, including hyperthyroidism (including Graves disease), adrenal disorders, hypothyroidism, hypopituitarism, and thyroid cancer. Our team of experts uses state-of-the-art techniques in their diagnosis, including ultrasound imaging and blood tests. We also provide comprehensive management for the treatment and surgical procedures for various thyroid conditions.