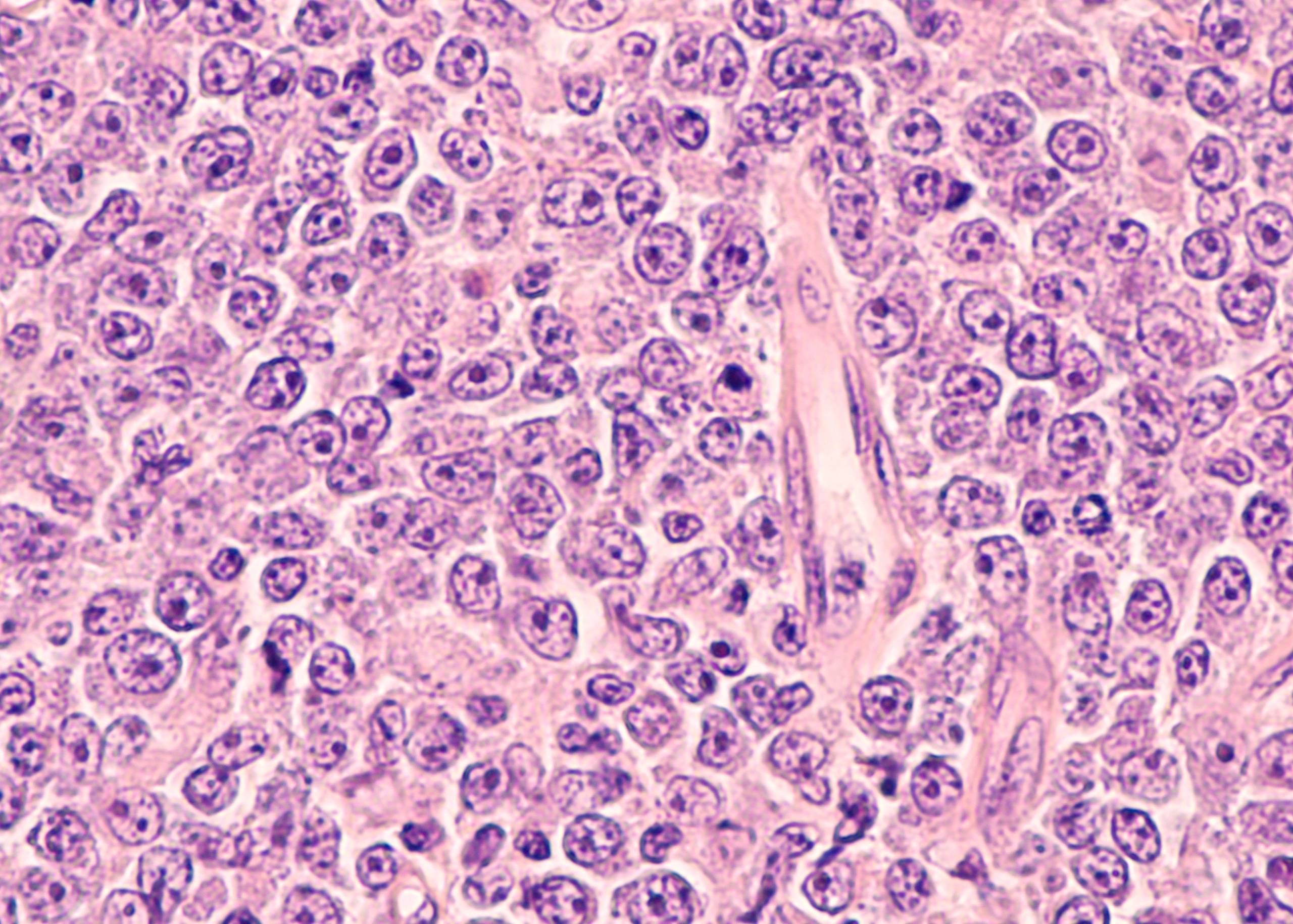
Cervical cancer is a disease of the cervix, which is a part of the female reproductive system. Changes in the cells of the cervix cause it. The cervix is made up of two parts: the endocervical canal and the exocervical or ectocervical region. The endocervical canal is lined with mucus-secreting epithelium and connects to the uterus (womb). The exocervical or ectocervical region has no tissue between it and the vagina (birth canal). Cancer can develop in either part of the cervix. The most common form starts at the surface layer of cells lining the exocervical or ectocervical area. This type is called squamous cell carcinoma and accounts for about 90% of all cervical cancers. The other 10% start at deeper levels in this area, where they are harder to detect because they don’t show up on routine Pap tests or visual examinations by doctors during pelvic examinations.
Symptoms of Cervical Cancer
There are a number of symptoms that may indicate cervical cancer in women. These include:
- Discharge from the vagina
- Bleeding between periods or after sex
- Pain during intercourse
- Feeling of pressure in the pelvis or lower back
- Pain in legs or pelvis
- Painful urination
Causes and Risk Factors of Cervical Cancer
It is caused by changes to the DNA in cervical cells. The main risk factor is human papillomavirus (HPV).
HPV is a common virus that can infect the skin and mucous membranes, including those of the cervix. Most people with HPV do not develop symptoms or health problems from it.
However, over time some women with persistent HPV infections may develop cervical cancer. It can also be caused by other factors, including:
Smoking increases your risk of developing cervical cancer and other types of cancers.
Having a weakened immune system: If you have an immune deficiency or have undergone organ transplantation surgery, the risk of developing cervical cancer is higher than average.
Prevention of Cervical Cancer
The best way to prevent cervical cancer is to get your Pap test and HPV vaccine on schedule, and to have regular checkups with your doctor.
Diagnosis
The diagnosis of cervical cancer is made by a combination of physical examination and laboratory tests. The doctor will perform a pelvic examination to look for any abnormalities, including lumps or discharge. In addition, he or she may perform a Pap test to look for abnormal cells in the cervix. If these tests are inconclusive, additional tests may be performed.
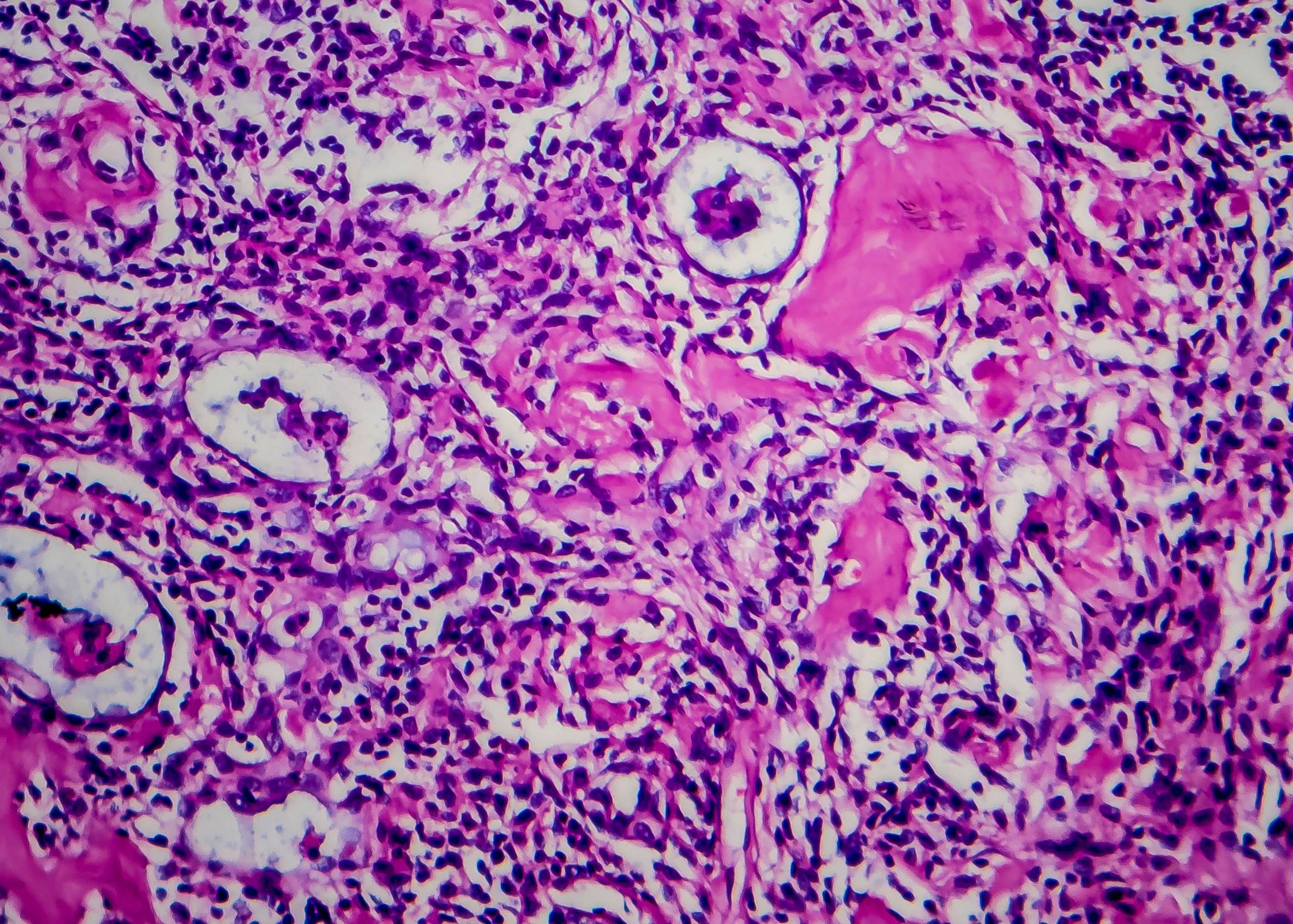
The following are common methods used to diagnose cervical cancer: Pap smear: A sample of cells from the cervix is collected with a brush or spatula and examined under a microscope for abnormalities; this helps determine if further testing is needed.
Colposcopy: A device called a colposcope is used to magnify the cervix; this allows the doctor to see any abnormal areas more clearly.
Endocervical Curettage: A small amount of tissue from the lining of the uterus (endocervix) is removed with a spoon-shaped instrument called a curette; this is done when other tests are not conclusive enough to determine if there are abnormal cells present on the surface of your cervix.
Laser Biopsy: This procedure uses high-intensity light energy (laser) to remove suspicious areas that may contain cancerous cells from your cervix.
Treatment
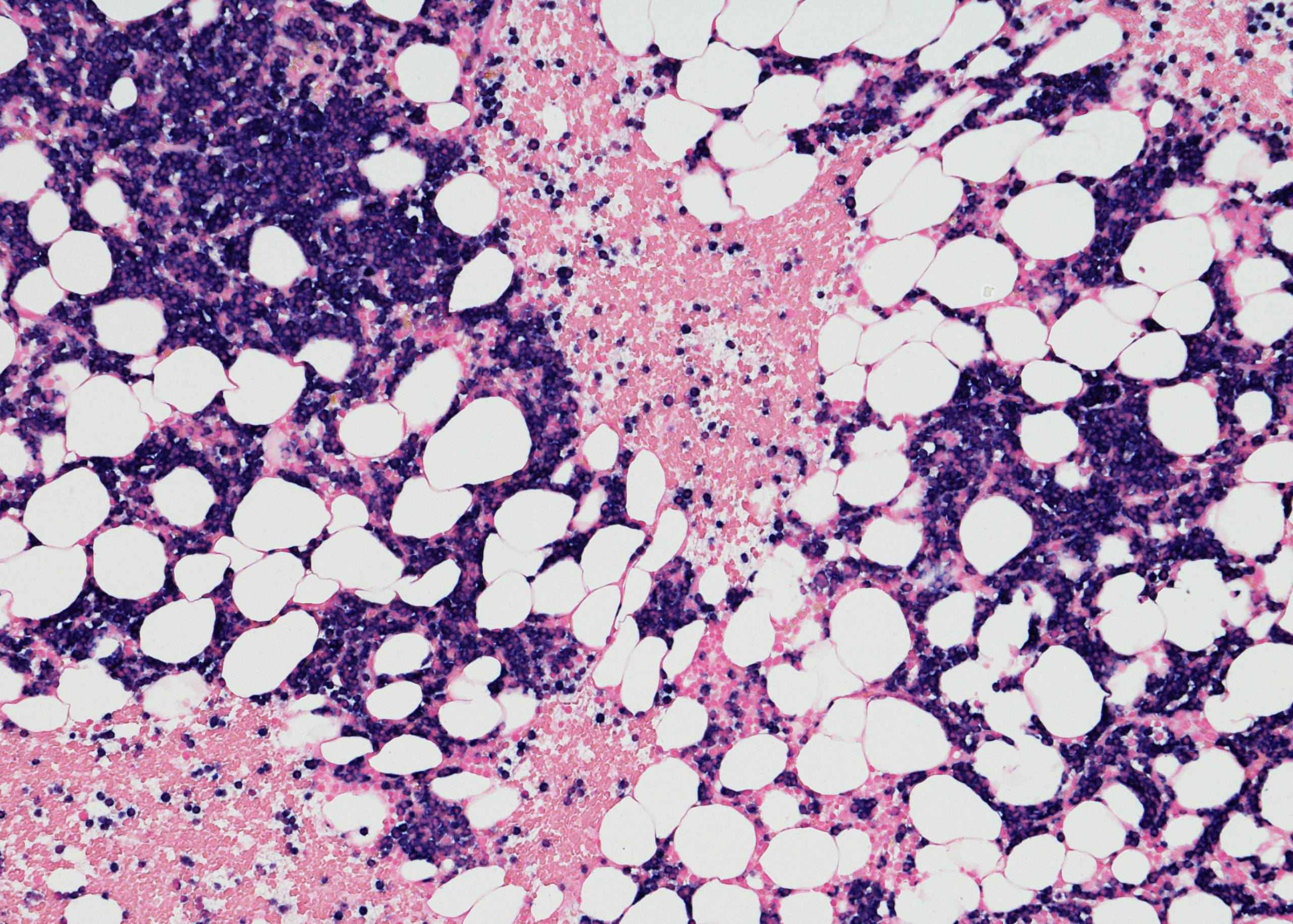
The treatment of cervical cancer depends on the stage at which it is diagnosed. If a precancerous lesion (called dysplasia) is detected, it can be treated with laser ablation or cryotherapy. If the cancer is discovered at an early stage, it can be treated with surgery to remove the cancerous tissue and surrounding lymph nodes, as well as chemotherapy and radiation therapy.
Advanced cervical cancer can be treated with chemotherapy, radiation therapy, and/or surgery. Surgical options include radical hysterectomy (removal of the uterus), radical trachelectomy (removal of uterus plus cervix), radical parametrectomy (removal of uterus plus upper part of vagina), and pelvic lymph node dissection (removal of lymph nodes).
We at Burjeel Medical City provide the best treatment for Cervical Cancer. We have a team of experienced gyneco-oncologists who are specialized in treating this disease. We also have the latest technology and equipment to ensure the best possible results.