Introduction
Burjeel Medical City continues to lead the way in advanced surgical interventions with a groundbreaking osseointegration procedure performed on a 57-year-old patient with a history of transtibial amputation. This innovative approach addresses common socket-related complications, offering improved mobility and quality of life for amputees facing chronic prosthetic challenges.
Patient History
The patient presented with significant socket-related issues stemming from a short residual limb. Years of conventional prosthetic use had resulted in thickening of the distal stump and callosity formation, despite previous skin grafting interventions. As a non-smoker with Type 2 diabetes, the patient represented a suitable candidate for this advanced surgical approach.
Clinical Assessment
Examination revealed clear evidence of soft tissue thickening and callosity at the distal end of the residual limb, consistent with chronic socket-related pressure and friction. The medical team noted healed graft sites on distal sections of the stump without any signs of active infection or ulceration, confirming candidacy for the procedure.
Surgical Approach
Under the expert guidance of a specialized surgical team including Dr. Munjed Al Muderis, Dr. Michael George Uglow, Dr. Ahmed Hammouda, and anesthesiologist Dr. Ahmed Omran, the osseointegration procedure was meticulously performed at Burjeel Medical City’s state-of-the-art surgical facility.
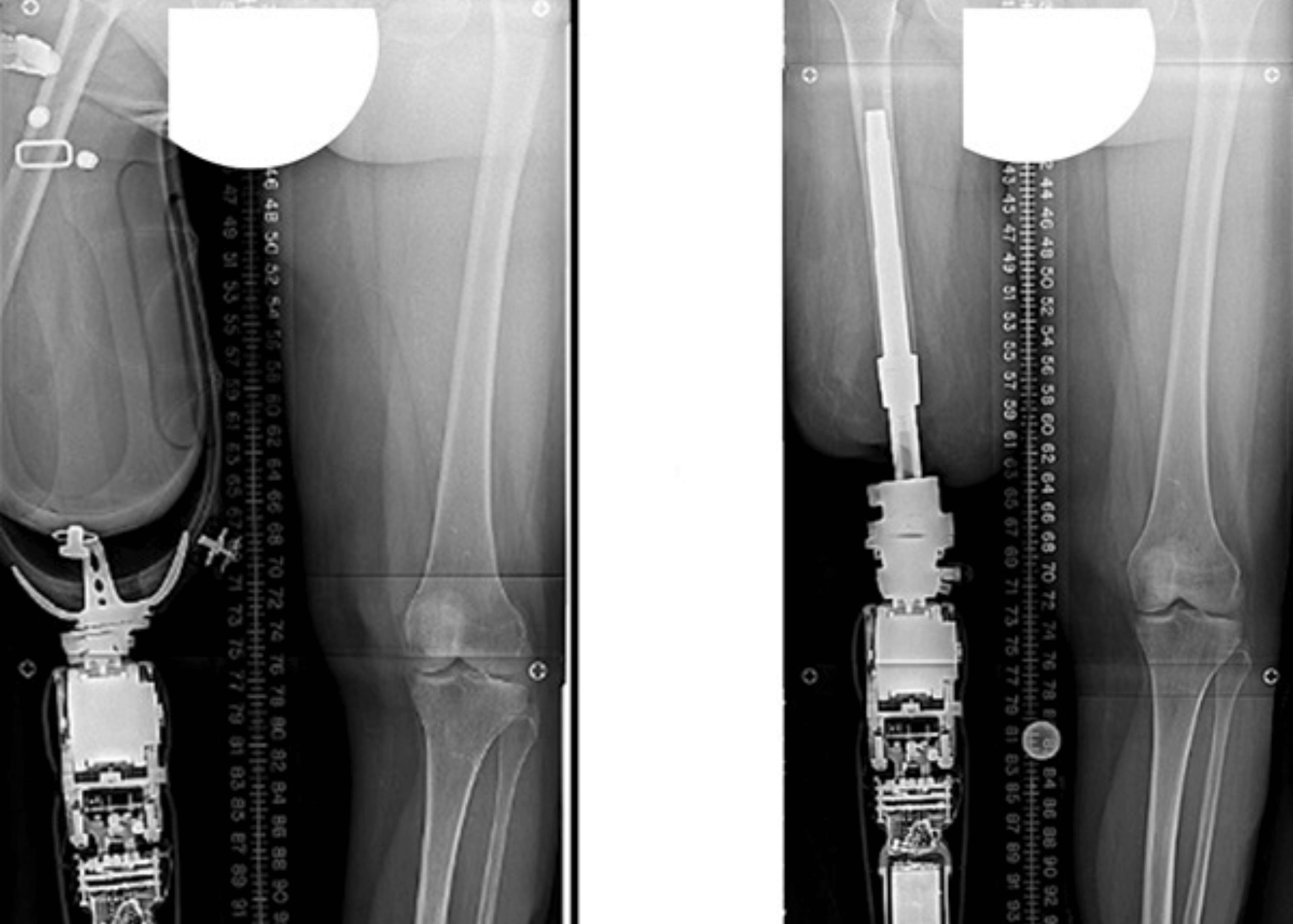
The surgical technique involved:
- Minimal skin incision using a corer to preserve tissue integrity
- Conservative soft tissue dissection to maintain stability and vascularity
- Preservation of posterior soft tissue and hyperkeratotic skin to minimize stoma infection risk
- Sequential reaming of the distal tibial medullary canal from 8mm to 23mm
- Fluoroscopy-guided broaching up to 24mm for precise implant positioning
- Insertion of an OPL Tibial Type D implant (24×80mm) with press-fit fixation
This approach achieved excellent rotational stability with minimal bleeding upon tourniquet release, eliminating the need for flap refashioning.
Benefits of Osseointegration
Osseointegration represents a revolutionary advancement for amputees facing challenges with traditional socket prosthetics. By directly anchoring the prosthetic limb to the bone, this technique eliminates common issues such as:
- Socket discomfort and pain
- Skin irritation and breakdown
- Limited range of motion
- Difficulty with prosthetic fitting
- Reduced proprioception and stability
Patients typically experience improved mobility, enhanced sensory feedback, and greater freedom from the limitations of socket-based systems.
Burjeel Medical City’s Advanced Surgical Capabilities
This procedure showcases Burjeel Medical City’s commitment to providing cutting-edge surgical interventions across its network of facilities in Abu Dhabi, Dubai, Al Ain, Sharjah, Al Dhafra, and Oman. With 70 operating rooms and specialized equipment including 7 catheterization laboratories, Burjeel Medical City’s surgical infrastructure supports complex procedures that transform patients’ lives.
Conclusion
The successful osseointegration procedure demonstrates the advanced surgical capabilities available at Burjeel Medical City facilities. By embracing innovative techniques, the team of orthopedic surgeons continues to provide life-changing solutions for patients with complex medical challenges, maintaining Burjeel Medical City’s position at the forefront of healthcare excellence in the region.