Teaching basic first aid skills.
Junior First Aiders


Teaching basic first aid skills.

A fun, hands-on activity where kids learn to build a balanced meal using food models.

Learning about body organs by assembling a life-sized puzzle.

As we age, our bodies undergo numerous changes, many of which can affect our bones. One of the most common conditions affecting bone health is osteoporosis—a silent disease that weakens bones, making them more prone to fractures. While osteoporosis can affect anyone, it is more prevalent among postmenopausal women, elderly individuals, and people with certain medical conditions.
Osteoporosis is a condition that results in weakened bones, increasing the risk of fractures, especially in the hips, spine, and wrists. The word “osteoporosis” literally means “porous bone,” which reflects the loss of bone density and strength over time. This condition occurs when the creation of new bone doesn’t keep up with the removal of old bone, leading to a fragile skeletal structure.
Several factors can contribute to the development of osteoporosis, including:
Osteoporosis is often called the “silent disease” because most people are unaware they have it until they experience a fracture. However, there are some signs to watch for:
Osteoporosis is diagnosed through a bone density test, typically a dual-energy X-ray absorptiometry (DEXA) scan. This test measures the density of bones in your spine, hip, and other areas to assess your fracture risk.
While osteoporosis may not be entirely preventable, there are several steps you can take to protect your bones and reduce your risk:
If you have been diagnosed with osteoporosis, don’t lose hope. There are effective treatments available. Medications such as bisphosphonates, selective estrogen receptor modulators (SERMs), and hormone replacement therapy (HRT) can slow bone loss and reduce the risk of fractures. Your endocrinologist will help create a tailored plan to protect your bones and prevent further complications.
Osteoporosis is a serious but manageable condition. By adopting healthy lifestyle habits, staying informed about your bone health, and seeking early intervention, you can significantly reduce your risk of osteoporosis and maintain strong bones for life.
At Burjeel Hospital, we are committed to helping you achieve optimal health and wellness. If you are concerned about your bone health or want to learn more about osteoporosis, we encourage you to schedule a consultation with one of our specialists. Together, we can help you build stronger bones and lead a healthier, more active life.
You must carefully read the “Consumer Information Use and Disclaimer” below in order to understand and correctly use this
information.
What is obesity?
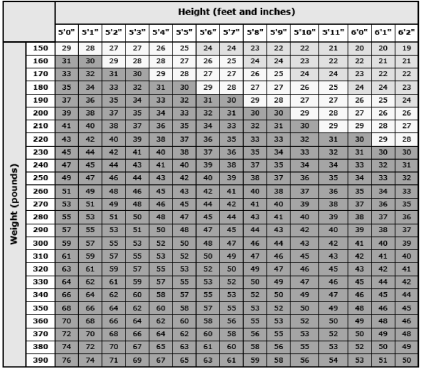
Doctors define obesity based on a person’s “body mass index,” or “BMI.” For adults, weight and height
are used to calculate BMI (figure 1).
For people who are White, Hispanic, or Black:
● “Overweight” means a BMI between 25 and 29.9.
● “Obesity” means a BMI of 30 or greater.
For people who are Asian, the cutoff numbers are a little different:
● “Overweight” means a BMI between 23 and 25.
● “Obesity” means a BMI of 25 or greater.
In addition to figuring out your BMI, your doctor might also measure around your belly. This is called
“waist circumference.” Doctors call it “central obesity” when people carry extra weight in the belly area,
even if their BMI is normal.
Obesity increases the risks of many different health problems. It can also make it harder for you to
move, breathe, and do other activities.
What are the health risks of obesity? —
Having obesity increases a person’s risk of developing many health problems. Here are just a few
examples:
● Diabetes
● High blood pressure
● High cholesterol
● Heart disease (including heart attacks)
● Stroke
● Sleep apnea (a disorder that makes you stop breathing for short periods while asleep)
● Asthma
● Cancer
18/09/2024, 11:28 Patient Education – UpToDate® Lexidrug™
https://online.lexi.com/lco/action/pcm 1/4
Does having obesity shorten a person’s life? —
Yes. Studies show that:
● People with obesity die younger than people who are a healthy weight.
● The risk of death goes up the heavier a person is. The degree of increased risk depends on how long the person has had obesity, and on what other medical problems they have.
People with central obesity (extra weight in the belly area) might also be at risk of dying younger.
Can medical treatments help me lose weight? —
Yes. There are medicines and surgery to help with weight loss. These treatments are meant for people
who have not been able to lose weight through lifestyle changes such as diet and exercise.
Weight loss treatments do not take the place of diet and exercise. People who have the treatments
must also change how they eat and how active they are.
How can I prevent the problems caused by obesity? —
The best thing you can do is lose weight. But even if weight loss is not possible, you can improve your
health and lower your risk if you:
● Become more active – Many types of physical activity can help, including walking. You can start
with a few minutes a day, and add more as you get stronger and build up your endurance.
Anything that gets your body moving is good for you. It is easier to create a habit if you choose
activities you enjoy.
● Improve your diet – It is healthy to have regular meal times, eat smaller portions, and not skip
meals. Limit sweets, and avoid processed foods. Try to eat more vegetables and fruits instead. The
best weight loss plans help you have a healthy view of eating.
● Quit smoking (if you smoke) – Some people start eating more after they stop smoking, so try to
make healthy food choices. Even if it increases your appetite, quitting smoking is still one of the
best things you can do to improve your health.
● Limit alcohol – For females of any age, limit alcohol to no more than 1 drink a day. For males 64
and younger, limit alcohol to no more than 2 drinks a day. For males 65 and older, limit alcohol to
no more than 1 drink a day.
Keeping a diary might help you reach your daily goals. You can use a paper diary or app to help you
record:
● What you eat and drink
● Your physical activity
● Your weight
What causes obesity? —
Your genes affect your risk of obesity. But lifestyle also has a big impact. You can develop obesity if you
eat too much, eat unhealthy foods, move too little, and watch a lot of TV.
There are other things that seem to increase the risk of obesity that you might not know about. Here
are some:
● Mother’s habits during and after pregnancy – People who eat a lot of calories, have diabetes, or
smoke during pregnancy have a higher chance of having babies who have obesity as adults. Also,
babies who drink formula might be more likely than breastfed babies to develop obesity later in
life.
● Habits and weight gain during childhood – Children or teens who are overweight or have obesity
are more likely to have obesity as an adult.
● Sleeping too little – People who do not get enough sleep are more likely to develop obesity.
● Taking certain medicines – Long-term use of certain medicines can cause weight gain. If you are
concerned that one of your medicines might be making you gain weight, talk to your doctor or
nurse. They might be able to switch you to a different medicine.
● Certain hormonal conditions – Some hormonal problems can increase the risk of developing
obesity. For example, hypothyroidism can cause weight gain, along with other symptoms.
What if I want to get pregnant? —
If you are overweight or have obesity, it might be harder to get pregnant. For males, obesity can also
cause sex problems, like having trouble getting or keeping an erection. This is more likely if you also
have high blood pressure or diabetes.
What if my child has obesity? —
In children, obesity has many of the same risks as it does in adults. For example, it can increase the risk
of diabetes, high blood pressure, asthma, and sleep apnea. It can also cause added problems related to
childhood. For example, obesity can make children grow faster than normal and cause girls to go
through puberty earlier than usual.
When should I call the doctor? —
Call your doctor or nurse if you want to try to lose weight. They can help you do it in a healthy way.
It can also help to work with a dietitian (food and nutrition expert). They can help you choose healthy
foods and plan meals.
All topics are updated as new evidence becomes available and our peer review process is complete.
This topic retrieved from UpToDate on: Jul 13, 2024.
Find your height (in feet and inches) in the top row. Then, find your weight (in pounds) in the first
column. Now, find where the column for your height and the row for your weight meet. That is your
BMI. For example, if you are 5-feet-9-inches tall and you weigh 260 pounds, your BMI is 38.
Graphic 62886 Version 4.0
Consumer Information Use and Disclaimer:
Disclaimer: This generalized information is a limited summary of diagnosis, treatment, and/or
medication information. It is not meant to be comprehensive and should be used as a tool to help the
user understand and/or assess potential diagnostic and treatment options. It does NOT include all
information about conditions, treatments, medications, side effects, or risks that may apply to a specific
patient. It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or
treatment of a health care provider based on the health care provider’s examination and assessment of
a patient’s specific and unique circumstances. Patients must speak with a health care provider for
complete information about their health, medical questions, and treatment options, including any risks
or benefits regarding use of medications. This information does not endorse any treatments or
medications as safe, effective, or approved for treating a specific patient. UpToDate, Inc. and its
affiliates disclaim any warranty or liability relating to this information or the use thereof. The use of this
information is governed by the Terms of Use, available at
https://www.wolterskluwer.com/en/know/clinical-effectiveness-terms. 2024© UpToDate, Inc. and its
affiliates and/or licensors. All rights reserved.
© 2024 UpToDate, Inc. and/or its affiliates. All rights reserve
Breast cancer is one of the most common cancers affecting women globally. The good news is that when detected early, it can be treated successfully. Early detection plays a vital role in improving survival rates, which is why it’s important for every woman to know the signs and symptoms of breast cancer and stay vigilant about her breast health.
Breast cancer doesn’t usually cause pain or noticeable symptoms in its earliest stages, making regular screening and awareness crucial. When caught early, breast cancer treatment is often more effective and less invasive, with higher survival rates. That’s why self-awareness and routine medical checkups are key to catching breast cancer before it spreads.
Breast cancer can present itself in a variety of ways. It’s important to know your body and recognize changes. Here are some common signs that may indicate early breast cancer:
1. Lump or Mass in the Breast:
One of the most common symptoms of breast cancer is the presence of a lump or mass in the breast. This mass is often hard and painless, but in some cases, it can feel tender or soft. Not all lumps are cancerous, but if you find one, it’s critical to consult your doctor for further evaluation.
2. Changes in Breast Size or Shape:
Noticeable changes in the size or shape of one breast compared to the other can be an early indicator of breast cancer. Sudden swelling, shrinkage, or asymmetry should not be ignored.
3. Skin Changes on the Breast:
Breast cancer can sometimes cause changes to the skin covering the breast, including:
4. Nipple Changes:
Nipple changes are another potential warning sign of breast cancer. Keep an eye out for:
5. Unexplained Breast Pain:
While breast pain is more commonly associated with hormonal changes, persistent or unusual pain in one area of the breast that doesn’t go away with your menstrual cycle could be a sign of something more serious.
6. Lumps in the Armpit:
Breast cancer can spread to nearby lymph nodes, including those in the armpit area. If you notice any unusual swelling or lumps in your armpit, it’s important to bring this to your doctor’s attention.
There are several steps you can take to ensure breast cancer is detected at its earliest and most treatable stage:
1. Perform Regular Breast Self-Exams
Knowing what’s normal for your breasts can help you detect changes early. A breast self-exam should be done monthly, ideally a few days after your period ends. Here’s how to perform a self-exam:
2. Get Regular Mammograms
Mammograms are the most reliable method for detecting breast cancer in its early stages. Most women should start having mammograms at age 40, but if you have a family history of breast cancer or other risk factors, your doctor may recommend starting earlier.
Mammograms can detect tumors before they’re large enough to feel and can identify abnormal areas that need further investigation. Make sure to schedule a mammogram as part of your regular health check-up.
3. Clinical Breast Exams
In addition to self-exams and mammograms, your OB-GYN or primary care physician should perform a clinical breast exam during your annual check-up. This is an important opportunity to discuss any changes you’ve noticed and receive a professional evaluation.
4. Genetic Testing for High-Risk Women
Women with a family history of breast cancer may benefit from genetic testing to determine if they carry BRCA1 or BRCA2 gene mutations, which increase the risk of breast and ovarian cancers. If you’re identified as high-risk, your doctor may recommend more frequent screenings or preventive measures.
While some risk factors for breast cancer, such as age and family history, are out of your control, there are several lifestyle choices you can make to reduce your risk:
Early detection of breast cancer is critical for successful treatment, and staying informed about the early warning signs can make all the difference. Be proactive about your breast health—perform regular self-exams, schedule routine mammograms, and maintain a healthy lifestyle.
At Burjeel Hospital, our team of experts is dedicated to providing comprehensive care for women. If you have concerns about your breast health or want to schedule a screening, our experienced doctors are here to guide you through the process with compassion and expertise.

Your heart is the core of your health, and taking steps to care for it can lead to a longer, healthier life. Dr. Kaes, a renowned cardiologist at Burjeel Al-Asharej, shares his expert tips for maintaining heart wellness:
By incorporating these practices into your daily life, you can enhance your heart health and overall well-being. Dr. Kaes and the team at Burjeel Al-Asharej are dedicated to helping you maintain a healthy heart for a vibrant life.

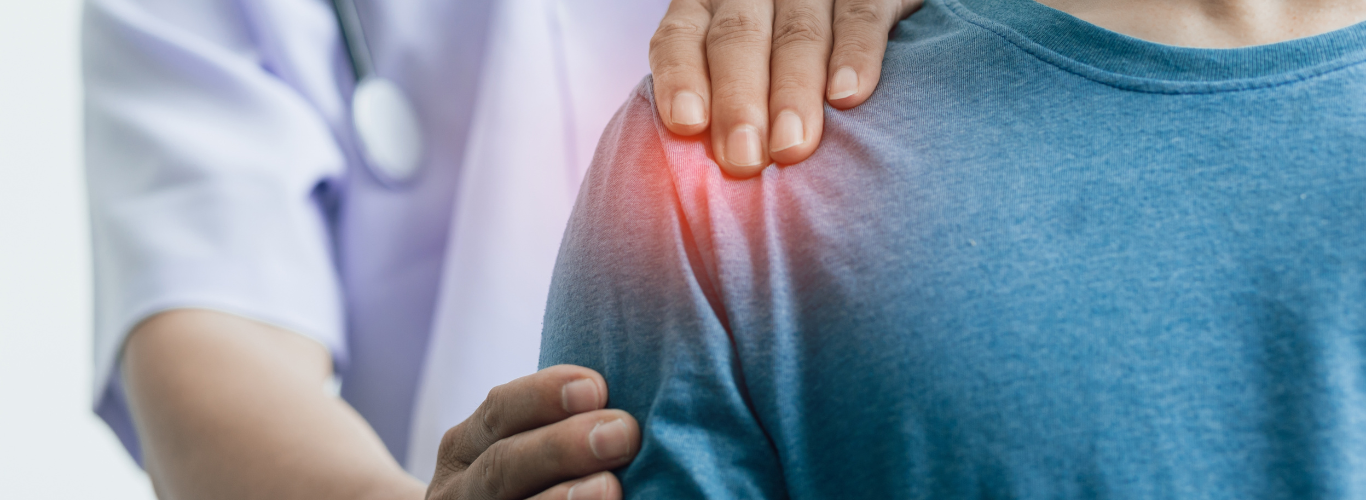
“Thanks to God, the pain has completely disappeared, and I have been able to return to my daily routine.”
For several years, Ms. Fatema Al Shehhi had been suffering from chronic lower back pain that radiated down her leg. The pain worsened with movement and caused muscle spasms, significantly impacting her quality of life. Despite trying various conservative treatments, her symptoms persisted. An MRI showed lumbar disc degenerative changes, diffuse disc bulges, and disc protrusions with nerve compression. To address the issue, Dr. Syed Kabir, Consultant Neurosurgeon at Burjeel Hospital Abu Dhabi Al Najda, performed a minimally invasive procedure called Bilateral Radiofrequency Ablation with Caudal Epidural Injection.This targeted treatment is designed to reduce pain and inflammation by focusing on the specific nerves causing discomfort. The procedure involves using radiofrequency energy to heat and deactivate the affected nerves, providing relief from pain.
Following the procedure, Ms. Fatema experienced significant improvement in her symptoms. The pain that had plagued her for so long was greatly reduced. Dr. Syed Kabir and his team closely monitored her recovery and were thrilled to report that her symptoms had significantly improved, allowing her to return to her normal life. Ms. Fatema is greatly thankful to the medical team at Burjeel Abu Dhabi Al Najda for their dedication and support throughout her treatment.
This case highlights the power of minimally invasive procedures in treating various conditions.

As the new school year approaches, it’s essential to ensure your child is ready to tackle the challenges and adventures ahead. From establishing healthy routines to addressing medical concerns, here are some comprehensive tips to help your child transition smoothly into the new school year.
One of the most crucial aspects of preparing for school is establishing a consistent daily routine. Children thrive on predictability, so start setting a regular bedtime and wake-up time a few weeks before school begins. This helps regulate their internal clocks and ensures they get adequate sleep, which is vital for their growth, development, and academic performance.
Before school starts, schedule a comprehensive health checkup for your child. This should include:
Set up a quiet, well-lit area in your home where your child can focus on homework and studying. Ensure this space is free from distractions and equipped with all necessary supplies, such as pencils, paper, and a comfortable chair.
Nutrition plays a significant role in a child’s ability to learn and concentrate. Encourage balanced meals that include a variety of fruits, vegetables, whole grains, and lean proteins. Limit sugary snacks and drinks, which can lead to energy crashes and decreased focus.
Physical activity is essential for maintaining a healthy body and mind. Encourage your child to engage in at least an hour of physical activity each day, whether through organized sports, playground time, or simply playing outside.
Starting a new school year can be stressful for children. Talk to your child about their feelings and any anxieties they may have. Encourage open communication and reassure them that it’s normal to feel nervous. Teach them relaxation techniques, such as deep breathing or mindfulness, to help manage stress.
Discuss safety protocols with your child, such as crossing the street, dealing with strangers, and what to do in emergencies. Make sure they know how to contact you or another trusted adult if needed.
Ensure the school has up-to-date emergency contact information and any necessary medical details about your child, such as allergies or chronic conditions.
Gather all required school supplies early to avoid last-minute shopping stress. Involve your child in this process to help them feel excited and prepared for the new school year.
Help your child approach the new school year with enthusiasm and a positive mindset. Discuss the exciting opportunities to make new friends, learn new things, and participate in fun activities.
Preparing for the new school year involves more than just buying school supplies. It’s about creating a supportive environment that promotes your child’s physical, emotional, and mental well-being. By following these tips, you’ll help your child start the school year on a healthy, confident, and enthusiastic note.
Shoulder arthroscopy is a minimally invasive procedure used to inspect, diagnose, and treat problems inside the shoulder joint.
Shoulder arthroscopy can be used to perform various procedures, including:
A small incision is made around the shoulder joint, and a thin, tube-like instrument called an arthroscope is inserted through one of the incisions. This instrument contains a tiny camera that transmits images to a video monitor, providing a clear view of the inside of the shoulder joint. Based on the findings, the surgeon will perform various procedures.
Shoulder arthroscopy is a minimally invasive surgery that results in less postoperative pain and allows for a quicker return to daily life activities. please contact our orthopedic institute for more information and a consultation.