For some time now, have you had recurrent or permanent shoulder pain? Know that this is a frequent pain: the shoulder is the most mobile of our joints, involved in many daily activities. These pains usually occur in the second half of life but can also affect younger people. When this unpleasant sensation has been present for a longer period and is recurring, affecting your daily activities, it is time to consult an Orthopedic Surgeon.
The shoulder joint is made of 4 joints whose stability and movement depend on four tendons that form the rotator cuff (supraspinatus, infraspinatus, subscapularis, and teres minor). The various joints, tendons, muscles and bursa involved in the shoulder movement characterize the different types of shoulder pain.
If you’re concerned, here’s a detailed explanation of the symptoms and causes of shoulder pain and the surgical and non-surgical treatment options!
Symptoms of Shoulder Pain
Rupture of the Rotator Cuff
Symptoms of a rotator cuff tear depend on the cause of the tear. They are quite discreet, with limited arm abduction if it is a trophic rupture (spontaneous or following repetitive strain injuries). In the event of a traumatic rupture (following a force or violent shock), the symptoms are much more severe, with pain in the shoulder stump and maximum functional impotence.
Slap Shoulder Injury
The SLAP lesion usually produces pain in the shoulder with certain gestures or movements. Clicking sensations may also be felt in certain positions. Shoulder examination with a SLAP lesion shows pain anteriorly or laterally. The shoulder is more or less unstable, and the patient feels a loss of strength in the shoulder and arm, combined with a loss of speed when throwing.
Shoulder Tendonitis
Symptoms of shoulder tendonitis are a pain when extending the arm, getting worse over time. It can also be felt at rest. Sometimes this pain may be accompanied by swelling in the shoulder joint. In addition, the patient may feel a cracking sensation in the joint and stiffness and loss of strength in the arm.
Tendinitis of the Tendons of the Triceps / Biceps
Symptoms of biceps tendinitis include pain in the front of the shoulder joint that extends to the arm and aggravates when bending, stretching, or pressing the tendon. For triceps tendinitis, the pain is located at the back of the elbow.
Shoulder Instability
Symptoms of shoulder instability are sharp, disabling pain during everyday movement. The patient also feels giving way in the shoulder joint, accompanied by cracking/popping sounds.
Shoulder Osteoarthritis
The symptoms of shoulder osteoarthritis are discreet at the beginning of the pathology but intensify over time. The patient feels intermittent pain in the shoulder, especially during rotations, as well as temporary blockages of the joint, accompanied by cracking and progressive stiffness.
Acromioclavicular Arthritis
The symptoms of acromioclavicular osteoarthritis are pain radiating to the neck and the trapezius, present in a virulent way at night because of the prolonged lateral position. This pain is also felt during adduction movements. In addition, it is accompanied by a loss of mobility and disabling stiffness in daily life.
Shoulder Fracture (Humerus + Scapula)
Symptoms of a shoulder fracture include severe pain (occurring during trauma) and an audible cracking sound. Immediately, the patient feels a consequent decrease in shoulder mobility. The shoulder is deformed and swollen, and the pain continues, even at rest.
Clavicle Fracture
Symptoms of clavicle fracture are sharp pain and audible cracking upon trauma. The patient cannot lift or move his arm at all. The area around the collarbone is swollen and has a bump. Bleeding is present, signs of an open fracture.
Acromioclavicular Dislocation
The symptoms of an acromioclavicular dislocation are pain and functional impotence, accompanied by hematoma, swelling and deformity of the shoulder, with a protrusion – under the skin – of the clavicle. The pain is throbbing in chronic forms, with jumps and cracks.
Capsulitis of the Shoulder
Symptoms of capsulitis of the shoulder appear gradually. After the first painful phase, the joint stiffens, limiting the movements of daily life. Subsequently, when the pathology worsens, the pain becomes more intense, occurring even at rest and accompanied by blockage of the shoulder.
Causes of Shoulder Pain
Your shoulder pain can have many causes, including:
- The consequence of a trauma when the pain follows a sprain, a tear, a dislocation, a tendon rupture or a fracture
- Inflammation of the rotator cuff or the rotator cuff tear: this pathology is the most common cause of shoulder pain; it can develop through a natural wear effect linked to aging or following repeated overhead movements linked to a sport or your profession
- SLAP injury is one of the causes of shoulder pain in athletes who use their arms above their heads. It produces pain and limitation of sports activity.
- Shoulder instability caused by your sports practice: in fact, certain sports result in the appearance of shoulder instability, in particular those which involve throwing or arming (volleyball, tennis, throwing of javelin, etc.). Even if you are young and healthy, these activities can eventually lead to pain
- An inflammatory or degenerative pathology of the shoulder, such as osteoarthritis or rheumatoid arthritis
- Bursitis (inflammatory lesion of the bursae) or calcification of the tendons of the rotator cuff
Diagnosis of Shoulder Pain
Following your pain, you have decided to consult your doctor. A clinical examination of your shoulder is carried out to find the cause of your pain and make a diagnosis.
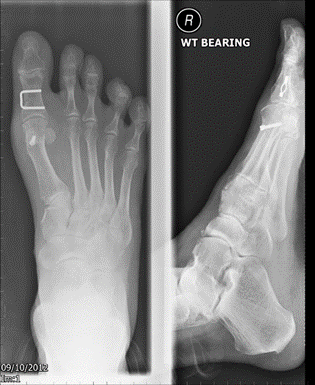
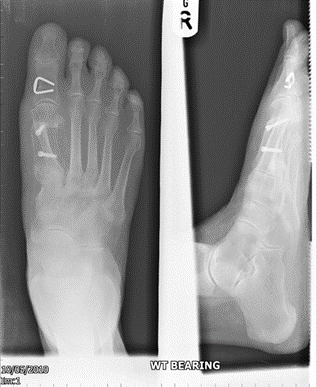
It starts with questioning to know the history and a clinical examination that gives an idea of the lesions that can explain the pain. Additional examinations are then carried out, in which a patient is certainly asked to perform x-rays. In some cases, ultrasound and MRI may be indicated. The imaging assessment confirms the diagnosis and guides towards the right treatment.
Treatment of Shoulder Pain
The initial form of treatment for shoulder pain is non-surgical. Conservative treatment consists of medications and physiotherapy. Exercises to improve shoulder mobility are also recommended. They are basically pendulum exercises and passive mobility of the shoulder and scapula. Despite intensive treatment, sometimes weeks to months go by in which patients do not entirely abandon the manifestation of discomfort and experience that the muscle impingement syndrome has improved. The treatment is based on the following three objectives:
- Restore joint function
- Regain all muscle strength
- Eliminate the pain
In certain cases where no improvement in pain is achieved from the aforementioned treatments of physiotherapy, mobility, medications, etc., surgical treatment may be recommended. In any case, the patient can help mitigate shoulder pain or get rid of it by following the guidelines indicated by the doctor at all times.
Surgical Treatment of Shoulder Pain
Shoulder surgery offers specific gestures according to the different ailments from which the shoulder joint suffers. It may be a rotator cuff tear repair, a total or reverse shoulder replacement, stabilization of the shoulder, etc. Each therapeutic objective defines an adequate surgical strategy.
Rotator Cuff Tear Repair
In a rotator cuff tear, tendons which allow the good mobility of the shoulder break following frequent friction against the bone of the acromion. The surgical operation is then an adequate restorative solution in which the patient undergoes an arthroscopic repair of the shoulder tendons.
A rotator cuff repair surgery involves docking the ruptured tendon at its natural location around the head of the humerus. This gesture is performed under arthroscopy, i.e. without opening the shoulder joint.
Arthroscopy respects all the anatomical structures and allows access to the joint without attacking the muscles. This technique has proven advantages over traditional surgery, such as minimized blood loss and accelerated post-operative recovery.
Several small incisions of 5mm each are made around the shoulder. An arthroscope, i.e. a small camera, is introduced through one of them to visualize the entire joint and, in particular, the ruptured tendon. Tiny instruments are introduced through the other incisions to perform the surgical procedure.
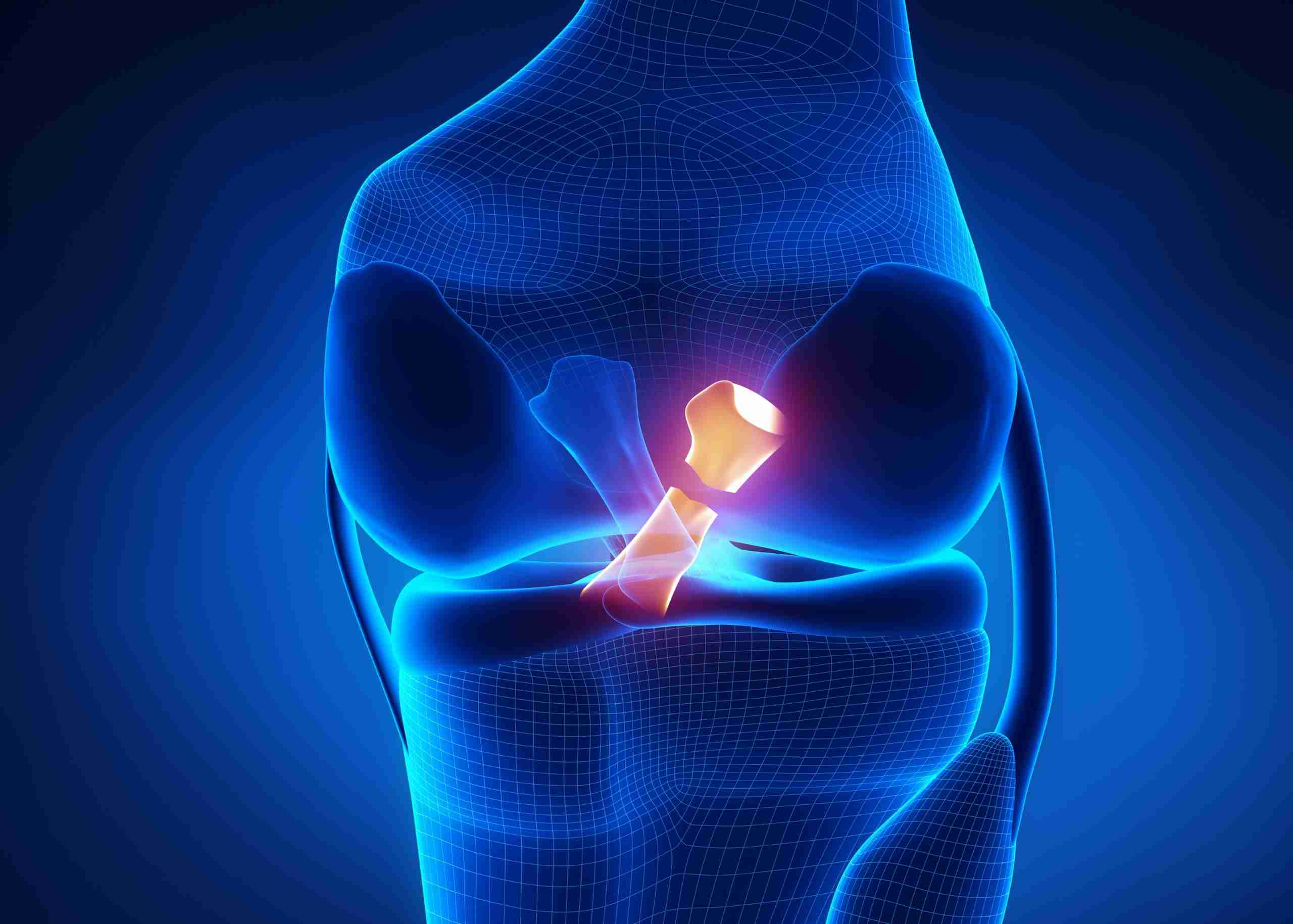
SLAP Lesion Repair
The evidence mentions SLAP Type II as the most difficult for arthroscopic repair. The patient with SLAP injury should be recommended a stage of Physiotherapy before and after surgery.
Although the surgical method is complex, labral tears must be repaired by arthroscopy, in which the labrum is re-anchored to the edge of the glenoid fossa.
Depending on the different types of SLAP tears and other factors (age, level of activity, other detected injuries, etc.), the surgeon identifies the best method to repair the SLAP tear after arthroscopic surgery. The method may require removing the torn part of the articular labrum or reattaching it using sutures. In some cases, suture repair is not required. Instead, the biceps tendon attachment is done to relieve shoulder pain.
Bicep Surgery
The practice of intensive sport sometimes leads to injuries, such as tendinopathy, that can go as far as the rupture of the biceps. This trauma requires biceps surgery to recover normal mobility.
Biceps surgery is performed by arthroscopy. The gesture depends on the type of lesion but is often that of tenotomy, more or less a tenodesis, depending on the patient’s age and activity. The tenotomy consists of performing a simple section of the long portion of the biceps, while Tenodesis involves fixing the tendon in place at the humerus level and removing its intra-articular part.
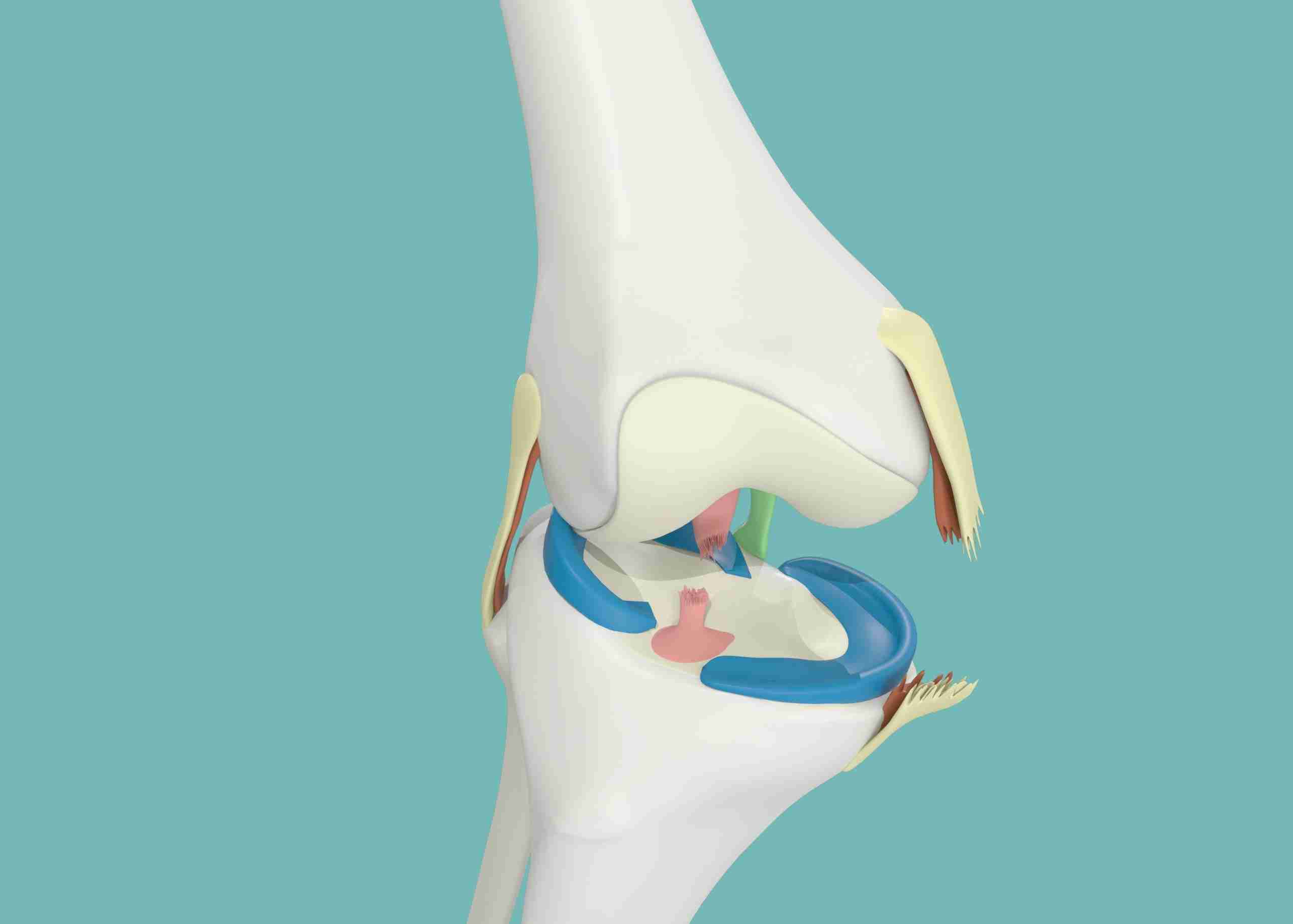
Reverse Total Shoulder Replacement and Total Shoulder Replacement Surgeries
A shoulder replacement surgery is recommended to treat shoulder osteoarthritis, which is the wear and tear of the cartilage, accompanied by changes in the bones of the humerus and the scapula, causing loss of mobility and pain. Since cartilage wear is irreversible, anti-inflammatories and painkillers may also end up being ineffective. This is when the question of surgery arises.
The shoulder replacement surgery aims to remove worn areas of bone and cartilage and replace them with artificial pieces.
A shoulder replacement surgery may be a total should prosthesis which respects all of the shoulder tendons in which the ball replaces the head of the humerus and articulates with the glenoid. The second case is the reversible total shoulder replacement when the tendons are ruptured, usually in older patients. The shape of this prosthesis makes it possible to actuate the deltoid muscle, which is present and functional in the vast majority of cases, making it possible to compensate for ruptured tendons.
Shoulder Hemiarthroplasty
Shoulder hemiarthroplasty involves replacing the diseased and degenerated part of the shoulder joint while leaving the functional one intact. Hemiarthroplasty meets the dual requirement of using minimal invasive techniques respecting the soft tissues (muscles, tendons and ligaments) and less voluminous implants, preserving the maximum of the patient’s bone.
Arthroscopy (Bankart Repair) for Shoulder Dislocation
Surgical treatment of shoulder instability is aimed at repairing and tightening the primary stabilizing structures of the shoulder to achieve a stable shoulder. It is usually performed by arthroscopic surgery. A repair of the anterior labral injury or Bankart injury and re-tensioning of the inferior glenohumeral ligament is performed. Bone anchors are used to achieve the fixation and tension of these structures.
Surgical treatment of shoulder instability has a high rate of good results with low risks of operative complications.
Arthroscopy for Acromioclavicular
Acromioclavicular stabilization surgery is recommended in patients with acromioclavicular dislocation. This involves returning the clavicle to its natural level arthroscopically. The principle is to lower the clavicle to connect it to the coracoid by a system of resistant threads tied together. However, the surgery can be complex if it is performed away from the trauma that requires replacing the ruptured ligaments with new ligaments.
If you or your loved one have recurrent or permanent shoulder pain and want to consult an Orthopedic Surgeon, contact the Burjeel Hospital for Advanced Surgery, Dubai. The Orthopedic Surgeons team at the Burjeel Hospital for Advanced Surgery has a distinguished history in complex surgical and nonsurgical procedures. Certified and Fellowship-trained, they are the leading experts in performing complex shoulder surgeries and treating all upper limb conditions. Call +971 800 55 or visit our website to book an appointment today!