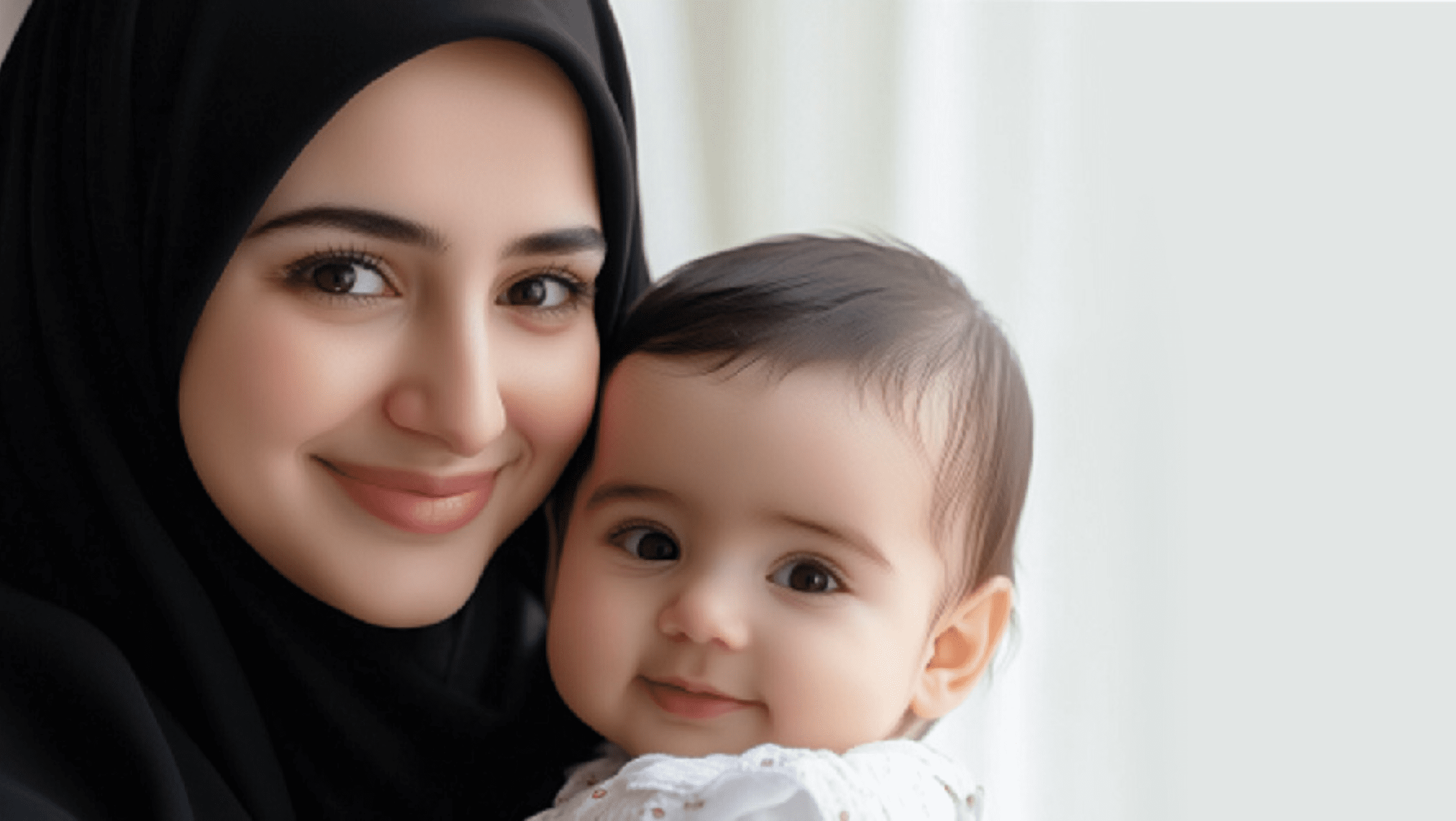
Breastfeeding is considered the optimal method of feeding an infant, offering numerous health benefits for both the mother and the baby. However, there are circumstances where formula feeding may be necessary. In this blog post, we will explore the benefits of breastfeeding and situations where formula might be needed, based on the guidance of Dr. Marwa Edrees, Obstetrics and Gynecology.
Benefits of Breastfeeding:
Health Benefits for the Baby:
- Nutrient-Rich: Breast milk contains the perfect balance of nutrients essential for a baby’s growth and development.
- Immune Support: Breast milk is rich in antibodies that help protect the baby from infections and illnesses.
- Digestive Health: Breast milk is easier for babies to digest compared to formula, reducing the risk of constipation and colic.
- Cognitive Development: Studies show that breastfeeding is linked to higher IQ scores in later childhood.
- Reduced Risk of Chronic Conditions: Breastfed babies have a lower risk of developing conditions such as asthma, obesity, and type 2 diabetes.
Health Benefits for the Mother:
- Postpartum Recovery: Breastfeeding helps the uterus contract and return to its pre-pregnancy size more quickly.
- Calorie Burning: Breastfeeding burns extra calories, which can help mothers lose pregnancy weight more easily.
- Reduced Risk of Certain Cancers: Long-term breastfeeding is associated with a lower risk of breast and ovarian cancer.
- Bonding: The physical closeness of breastfeeding enhances the emotional bond between mother and baby.
When to Use Formula:
While breastfeeding is highly recommended, there are certain situations where formula feeding may be necessary or preferred:
- Medical Conditions:
- Mother’s Health: If the mother has certain medical conditions or infections (e.g., HIV) that can be transmitted through breast milk, formula feeding may be recommended.
- Medications: Some medications taken by the mother can be harmful to the baby and may necessitate formula feeding.
- Low Milk Supply:
- Some mothers may struggle to produce enough milk despite their best efforts. Supplementing with formula can ensure the baby gets adequate nutrition.
- Returning to Work:
- While many workplaces support breastfeeding, some mothers may find it challenging to maintain their milk supply and may choose to use formula.
- Personal Choice:
- Some mothers may prefer formula feeding due to personal reasons or lifestyle considerations.
Conclusion:
Breastfeeding provides unparalleled benefits for both the mother and the baby, but formula feeding can be a valuable alternative in certain circumstances. It is important to make informed decisions based on individual needs and health conditions. Consulting with a healthcare professional, such as an Obstetrics and Gynecology or a pediatrician, can help mothers choose the best feeding method for their babies.