Imagine reaching for your morning coffee and suddenly your shoulder sounds like a rusty gate in an old sandstorm. Yes, we get you, not quite the way to start the day, and definitely not a sign to ignore. Those aches? They’re not just your body getting older. They’re warning signs your joints are sending an SOS. Osteoarthritis doesn’t just show up – it moves in like an uninvited guest, making simple things feel like a challenge. But here’s the thing: your body’s trying to tell you something. And we’re here to translate. In the next few minutes, we’ll break down the 10 signals your joints are desperately trying to communicate. No medical textbook mumbo-jumbo, just real talk about what’s happening inside you.
1. Understanding Osteoarthritis: A Brief Overview
What is osteoarthritis?
Osteoarthritis is a degenerative joint disease that occurs when the protective cartilage that cushions the ends of bones wears down over time. This condition can affect any joint in the body, but it most commonly impacts the knees, hips, hands, and spine.
Who is at risk for developing osteoarthritis?
Several factors can increase the risk of developing osteoarthritis:
- Age: The risk increases as we get older.
- Gender: Women are more likely to develop osteoarthritis, especially after menopause.
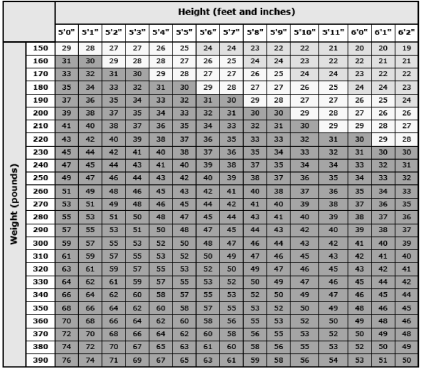
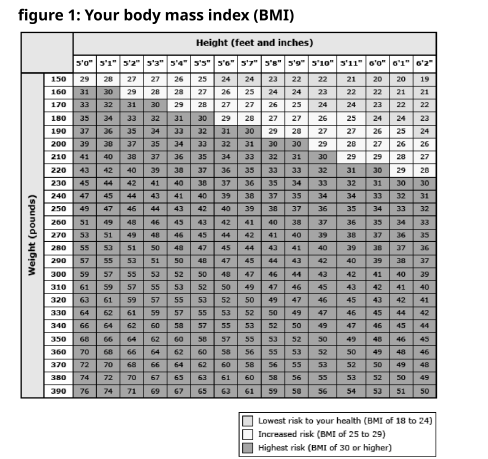
- Obesity: Excess weight puts additional stress on weight-bearing joints, often leading to knee pain or hip pain causes.
- Joint injuries: Previous injuries can lead to knee pain after exercise or hip pain dull ache later in life.
- Genetics: Some people inherit a tendency to develop osteoarthritis.
The importance of early detection and treatment
Recognizing the signs of osteoarthritis early is crucial for managing the condition effectively. Early detection allows for prompt treatment, which can help:
- Slow down the progression of the disease.
- Reduce pain and improve joint function.
- Maintain quality of life and independence.
- Prevent or delay the need for surgical interventions like knee pain treatment at home.
2. Joint Pain and Stiffness: The Primary Indicators
Persistent pain in affected joints
One of the most common signs of osteoarthritis is persistent pain in the affected joints, such as knee joint pain or hip joint pain. This pain may:
Start as a dull ache or burning sensation
Worsen over time, particularly during or after physical activity.
Morning stiffness and difficulty in movement
Many people with osteoarthritis experience stiffness, particularly in the lower back or knees:
- Stiffness often lasts less than 30 minutes.
- Symptoms may improve with lower back stretches or gentle movement.
Pain that worsens with activity or at the end of the day
As the day progresses, you might notice:
- Increased pain with prolonged activity
- Discomfort that peaks towards the end of the day
- Relief when resting the affected joint
3. Changes in Joint Flexibility and Range of Motion
Reduced joint flexibility
Osteoarthritis can lead to a decrease in joint flexibility, which may manifest as:
- Difficulty bending or straightening the affected joint
- A feeling of tightness or resistance when moving the joint
- Gradual loss of full range of motion over time
Difficulty in performing everyday tasks
As joint flexibility decreases, you might find it challenging to:
- Climb stairs or get in and out of a car
- Open jars or grip objects tightly
- Perform fine motor tasks like buttoning a shirt
Compensatory movements to avoid pain
To minimize discomfort, you might unconsciously develop new ways of moving, such as:
- Limping or favoring one leg over the other
- Using your hands differently to avoid stressing certain joints
- Relying more on unaffected joints to compensate for the painful ones
4. Swelling and Tenderness Around Joints
Visible swelling in affected areas
Swelling is a common sign of osteoarthritis, particularly in larger joints like knees and ankles. You might notice:
- A puffy or swollen appearance around the joint
- Increased size compared to the unaffected joint
- Swelling that comes and goes or persists over time
Warmth and tenderness to touch
Inflamed joints may feel warm to the touch and be tender when pressure is applied. This can include:
- A noticeable increase in temperature around the affected area
- Discomfort or pain when the joint is gently pressed
- Increased sensitivity in the surrounding skin
Soft tissue inflammation around joints
The soft tissues surrounding the affected joint may also become inflamed, leading to:
- A feeling of fullness or tightness in the joint area
- Reduced flexibility in the surrounding muscles and ligaments
- Visible changes in the contour of the joint
5. Bone Spurs and Joint Deformities
Formation of bone spurs
As osteoarthritis progresses, the body may try to repair the damage by creating bone spurs. These can:
- Cause additional pain and stiffness
- Be felt as hard lumps around the affected joint
- Show up on X-rays as small, bony projections
Changes in joint appearance
Over time, you might notice visible changes in the affected joints, such as:
- Enlarged or misshapen joints, particularly in the fingers
- Knobby appearances at the joint sites
- Asymmetry between corresponding joints on opposite sides of the body
Progressive joint misalignment
In advanced stages of osteoarthritis, joints may become misaligned, leading to:
- Visible deformities, such as bowlegs or knock knees
- Changes in gait or posture
- Increased difficulty in performing normal joint movements
6. Grating Sensation and Popping Sounds
Crepitus: crackling or grating sensations
Crepitus refers to the feeling or sound of grinding, crackling, or popping in a joint. You might experience:
- A sandpaper-like sensation when moving the joint
- A feeling of roughness or unevenness during joint movement
- Tactile vibrations that can be felt through the skin
Audible popping or clicking sounds
In addition to the sensation of crepitus, you might hear:
- Clicking or popping sounds when bending or straightening the joint
- Creaking noises during movement, especially in weight-bearing joints
- Sounds that become more noticeable as the condition progresses
When to be concerned about joint sounds
While some joint sounds are normal, it’s important to pay attention to:
- New or increased frequency of joint noises
- Sounds accompanied by pain or discomfort
- Changes in the type or volume of joint sounds
7. Muscle Weakness and Atrophy
Weakening of muscles around affected joints
Osteoarthritis can lead to weakening of the muscles surrounding the affected joints due to:
- Reduced use of the joint because of pain
- Changes in joint mechanics affecting muscle function
- Reflexive muscle inhibition as a protective mechanism
Visible muscle wasting
In some cases, you might notice:
- A decrease in muscle mass around the affected joint
- Visible thinning or flattening of muscle contours
- Asymmetry when comparing to the unaffected side
Impact on overall strength and stability
Muscle weakness associated with osteoarthritis can affect:
- Balance and coordination, increasing the risk of falls
- The ability to perform weight-bearing activities
- Overall functional capacity in daily life
8. Fatigue and Sleep Disturbances
Increased tiredness and fatigue
People with osteoarthritis often experience increased fatigue, which can be attributed to:
- Constant pain and discomfort
- Reduced physical activity and deconditioning
- The body’s ongoing inflammatory response
Difficulty sleeping due to joint pain
Osteoarthritis can significantly impact sleep quality:
- Pain may make it difficult to find a comfortable sleeping position
- Stiffness can cause discomfort when trying to fall asleep or upon waking
- Frequent nighttime awakenings due to pain can disrupt sleep cycles
The cycle of pain, poor sleep, and fatigue
A vicious cycle can develop:
- Pain leads to poor sleep
- Lack of quality sleep increases pain sensitivity
- Increased pain and fatigue further impact daily activities and sleep
9. Weather Sensitivity and Joint Pain
Increased pain during weather changes
Many people with osteoarthritis report that their symptoms worsen with certain weather conditions:
- Cold and damp weather often exacerbates joint pain
- Sudden changes in temperature or air pressure can trigger discomfort
- Some individuals experience increased pain before or during rainy weather
Humidity and barometric pressure effects
Specific weather factors that may influence osteoarthritis symptoms include:
- High humidity, which can increase joint inflammation
- Drops in barometric pressure, which may cause tissues to expand and put pressure on joints
- Rapid weather changes that don’t allow the body time to adjust
Seasonal variations in symptom severity
Some people with osteoarthritis notice patterns in their symptoms:
- Winter months often bring increased joint stiffness and pain
- Warmer, drier seasons may provide some relief
- Transitions between seasons can be particularly challenging
10. Psychological Impact and Mood Changes
Depression and anxiety related to chronic pain
Living with osteoarthritis can take a toll on mental health:
- Chronic pain can lead to feelings of helplessness and hopelessness
- Anxiety about future pain or disability is common
- The stress of managing a chronic condition can contribute to depression
Frustration with limited mobility
As osteoarthritis progresses, individuals may experience:
- Frustration with the inability to perform previously easy tasks
- Feelings of loss related to decreased independence
- Anger or resentment towards the limitations imposed by the condition
Social isolation due to osteoarthritis symptoms
The physical and emotional impacts of osteoarthritis can lead to:
- Withdrawal from social activities due to pain or mobility issues
- Reluctance to make plans due to unpredictable symptoms
- Feelings of loneliness or disconnection from others
Summary
Recognizing the signs of osteoarthritis is crucial for early intervention and effective management. The ten key signs to watch for include:
- Persistent joint pain and stiffness
- Changes in joint flexibility and range of motion
- Swelling and tenderness around joints
- Bone spurs and joint deformities
- Grating sensations and popping sounds
- Muscle weakness and atrophy
- Fatigue and sleep disturbances
- Weather sensitivity affecting joint pain
- Psychological impact and mood changes
- Social isolation due to symptoms
If you experience these symptoms, especially if they persist or worsen over time, it’s important to consult with a healthcare professional for proper diagnosis and treatment.
FAQs
Osteoarthritis can develop at any age, but it’s most common in people over 50. However, younger individuals can develop it due to factors like joint injuries or genetic predisposition.
While not all cases of osteoarthritis can be prevented, you can reduce your risk by maintaining a healthy weight, exercising regularly, protecting your joints during physical activities, and managing other health conditions that may contribute to joint damage.
Diagnosis typically involves a combination of physical examination, medical history review, and imaging tests such as X-rays or MRI scans. In some cases, blood tests or joint fluid analysis may be performed to rule out other conditions.
Treatment options include pain management (medications, topical treatments), physical therapy, lifestyle modifications, assistive devices, and in severe cases, surgical interventions like joint replacement.
Yes, regular exercise is generally recommended for people with osteoarthritis. Low-impact activities like swimming, cycling, and gentle stretching can help maintain joint flexibility, strengthen supporting muscles, and reduce pain. However, it’s important to consult with a healthcare professional to develop an appropriate exercise plan.