Introduction
Infective endocarditis is a serious infection of the endocardial surface of the heart, often affecting one or more heart valves. When complicated by septic shock, it presents a significant clinical challenge with high mortality rates, requiring prompt medical intervention and potentially emergent surgical management. This case study details the successful management of a complex case of septic shock and endocarditis in a 42-year-old male patient, marking a significant milestone as the first cardiac surgery performed at Burjeel Specialty Hospital, Sharjah.
Patient Presentation
A 42-year-old Filipino male presented to a non-Burjeel healthcare facility on April 4, 2024, with complaints of sudden-onset breathing difficulty that began at approximately 10:30 PM that same evening. Upon arrival at the emergency department, the patient was in a gasping state, unresponsive, and exhibiting concerning symptoms of desaturation and hypotension.
Initial Emergency Management
The severity of the patient’s condition necessitated immediate intervention. The emergency team promptly:
- Initiated endotracheal intubation to secure the airway
- Established inotropic support to stabilize blood pressure
- Began diagnostic workup to identify the underlying cause
Diagnostic Findings
The initial diagnostic evaluation resulted in a diagnosis of:
- Septic shock
- Cardiogenic shock
- Multi-organ failure
Further history revealed that the patient had been experiencing:
- Intermittent fever for three months
- Significant weight loss
- Known thyroid disease with no surgical history
Due to bed unavailability at the initial facility, the patient was transferred to Medeor Hospital the following day. There, additional diagnostic tests were performed.
Key Laboratory Findings
Laboratory tests demonstrated:
- Elevated white blood cell count
- Markedly elevated C-reactive protein (CRP)
- High procalcitonin levels, strongly suggestive of bacterial infection
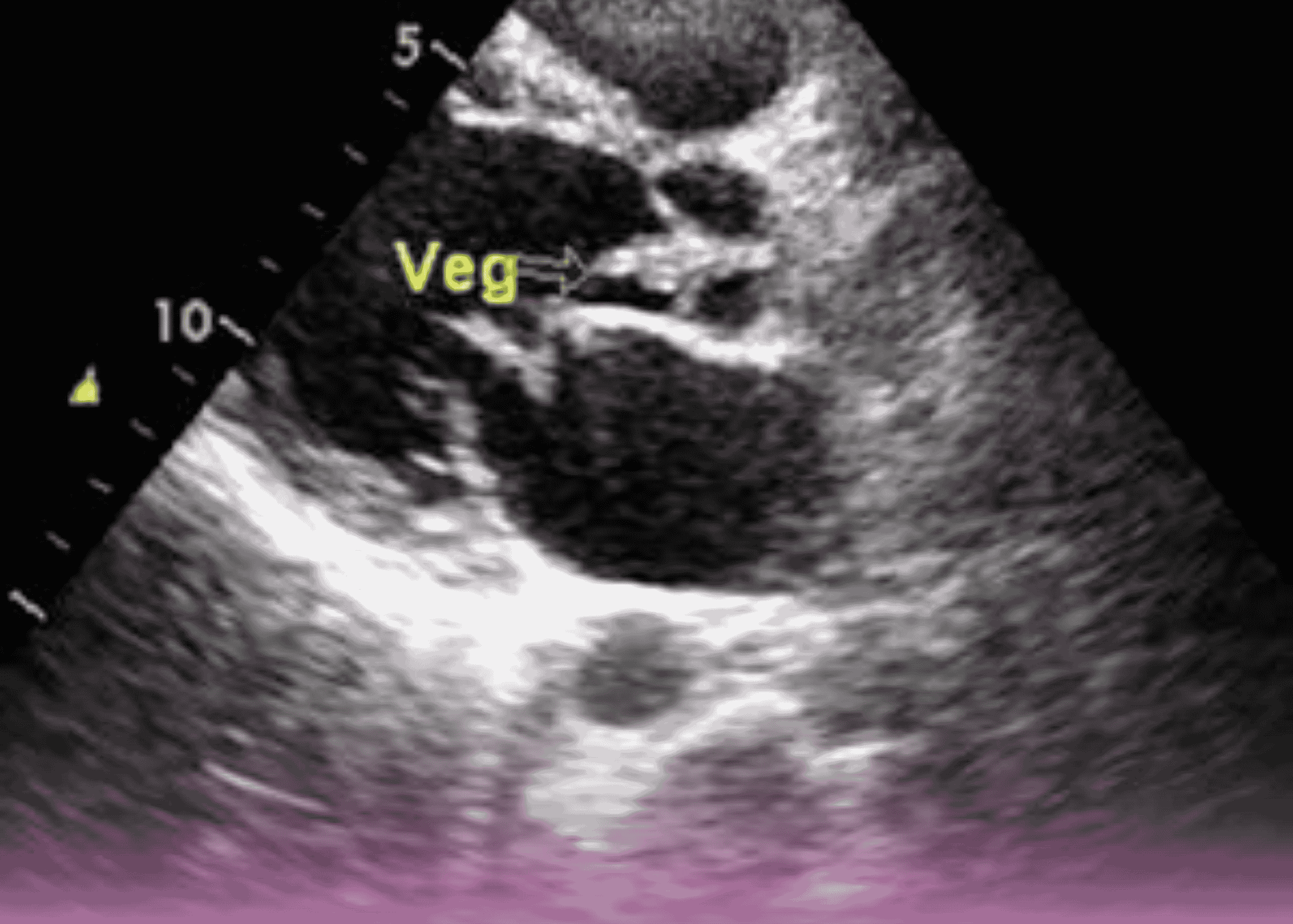
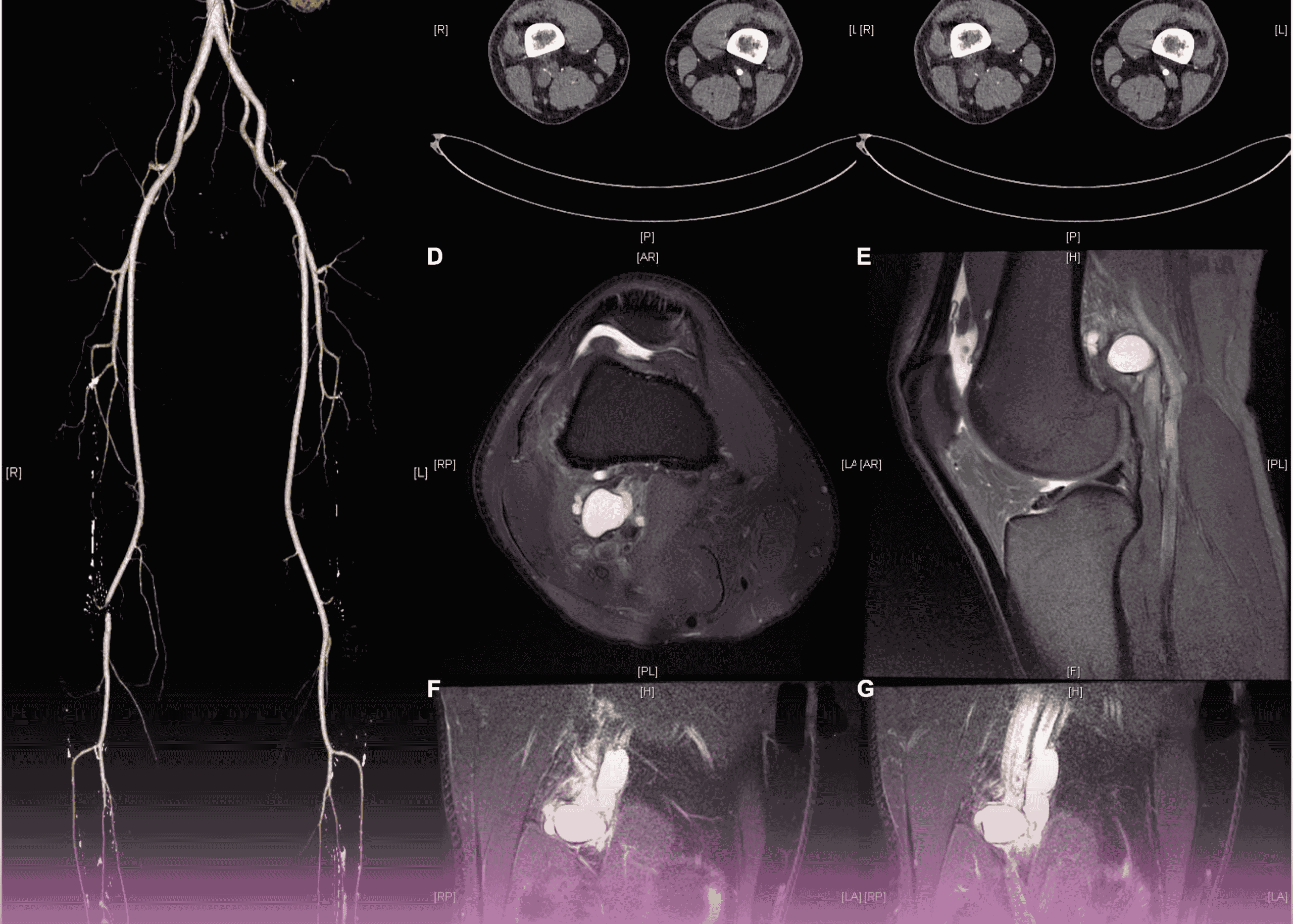
Imaging and Microbiological Results
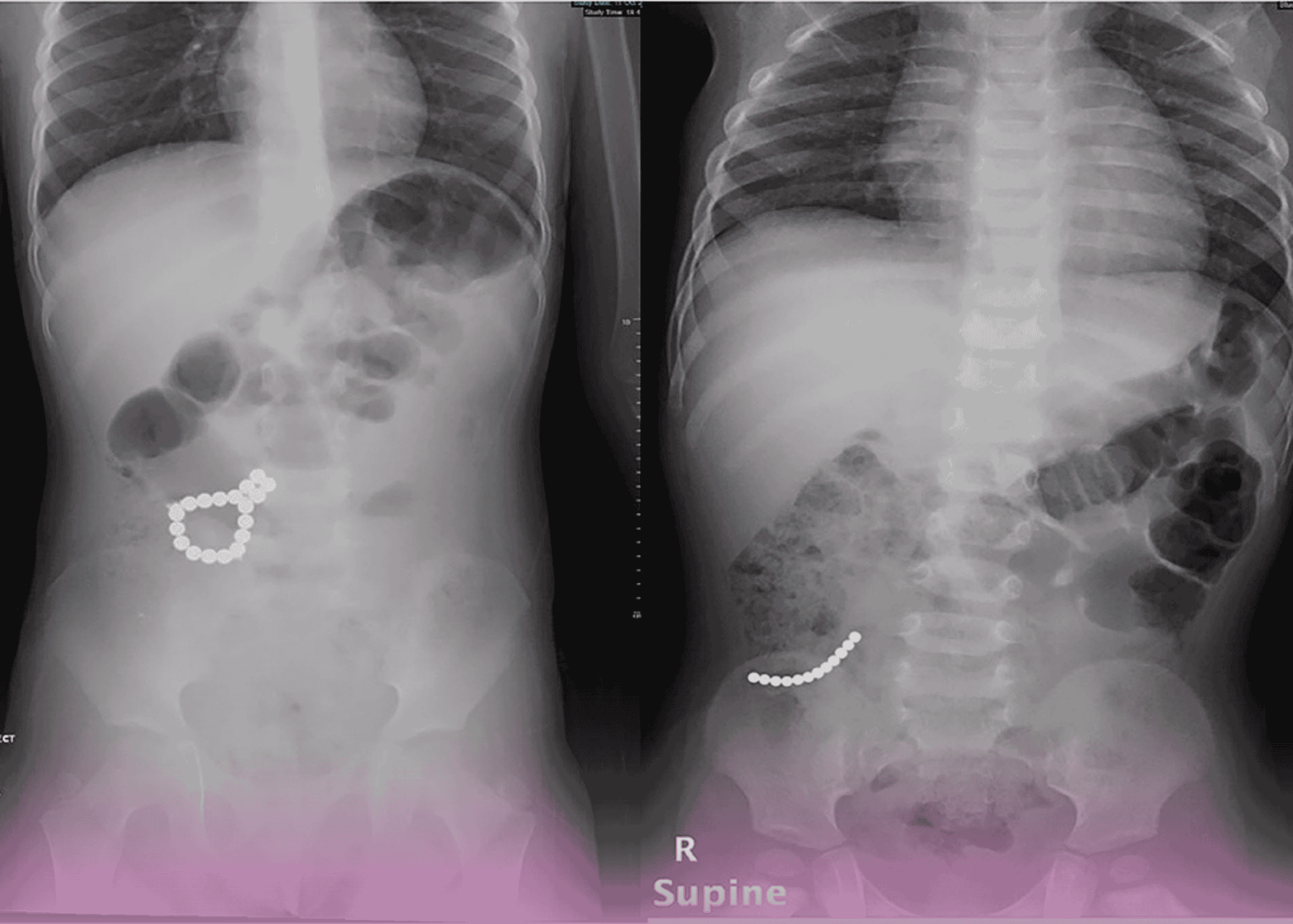
- 2D Echocardiography: Revealed large vegetation on the mitral anterior leaflet with severe mitral regurgitation
- Blood Cultures: Identified Streptococcus species from samples taken at the non-Burjeel facility
Comprehensive Diagnosis
Based on the clinical presentation and diagnostic findings, the patient was diagnosed with:
- Rheumatic Heart Disease
- Severe Mitral Regurgitation
- Infective Endocarditis
- Severe Pulmonary Arterial Hypertension (PAH)
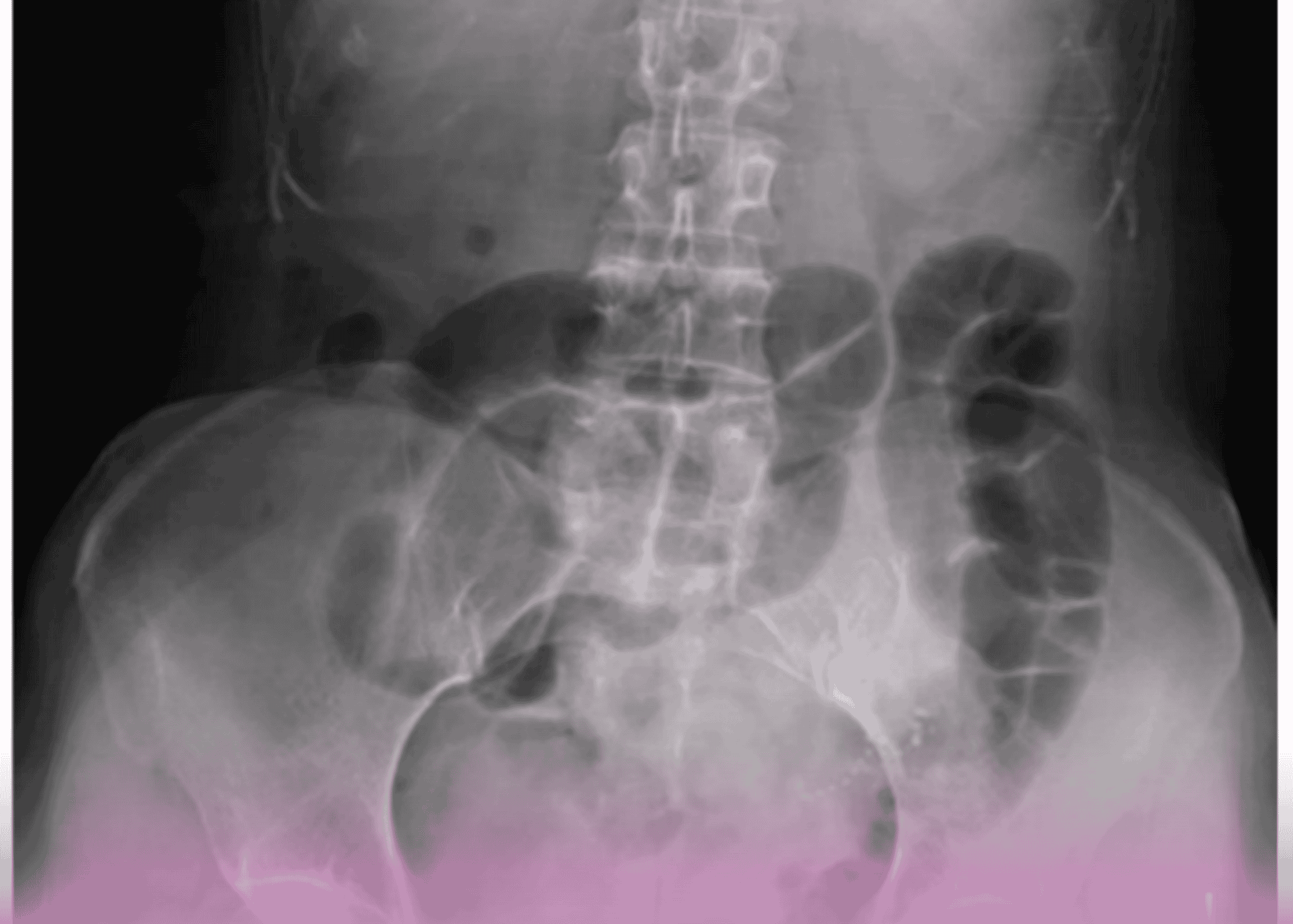
- Acute Kidney Injury (AKI)
Treatment Course
Initial Medical Management
The patient showed a positive response to antimicrobial therapy with:
- Vancomycin
- Linezolid
Within two weeks of initiating antibiotic therapy, the patient’s CRP levels normalized, indicating effective control of the infection. He was subsequently discharged home on oral Linezolid tablets.
Surgical Planning
Following stabilization and initial treatment of the acute infection, the patient was scheduled for mitral valve replacement at Burjeel Specialty Hospital, Sharjah. This procedure would represent a significant milestone as the first cardiac surgery to be performed at this facility.
Surgical Intervention
Procedure Details
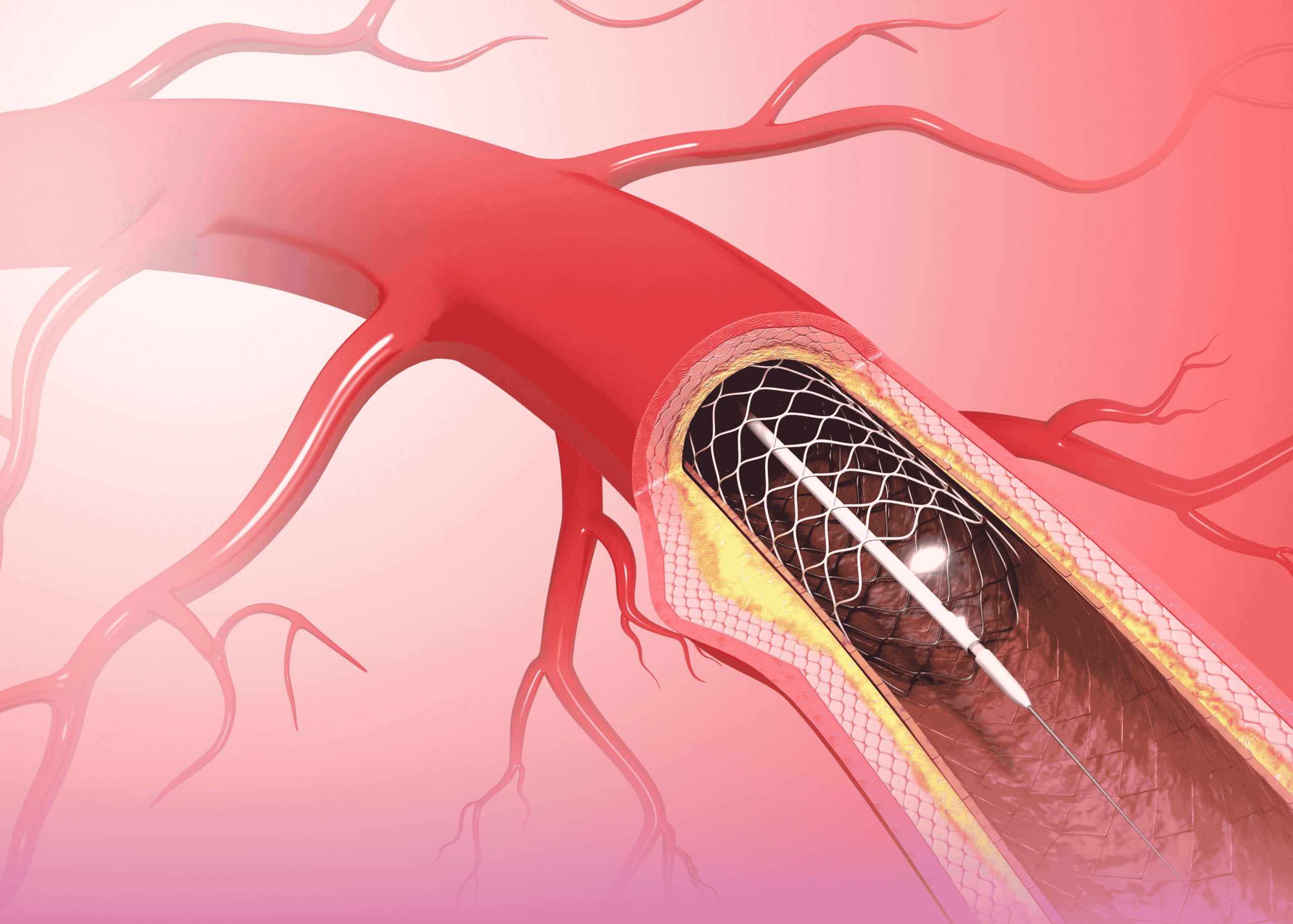
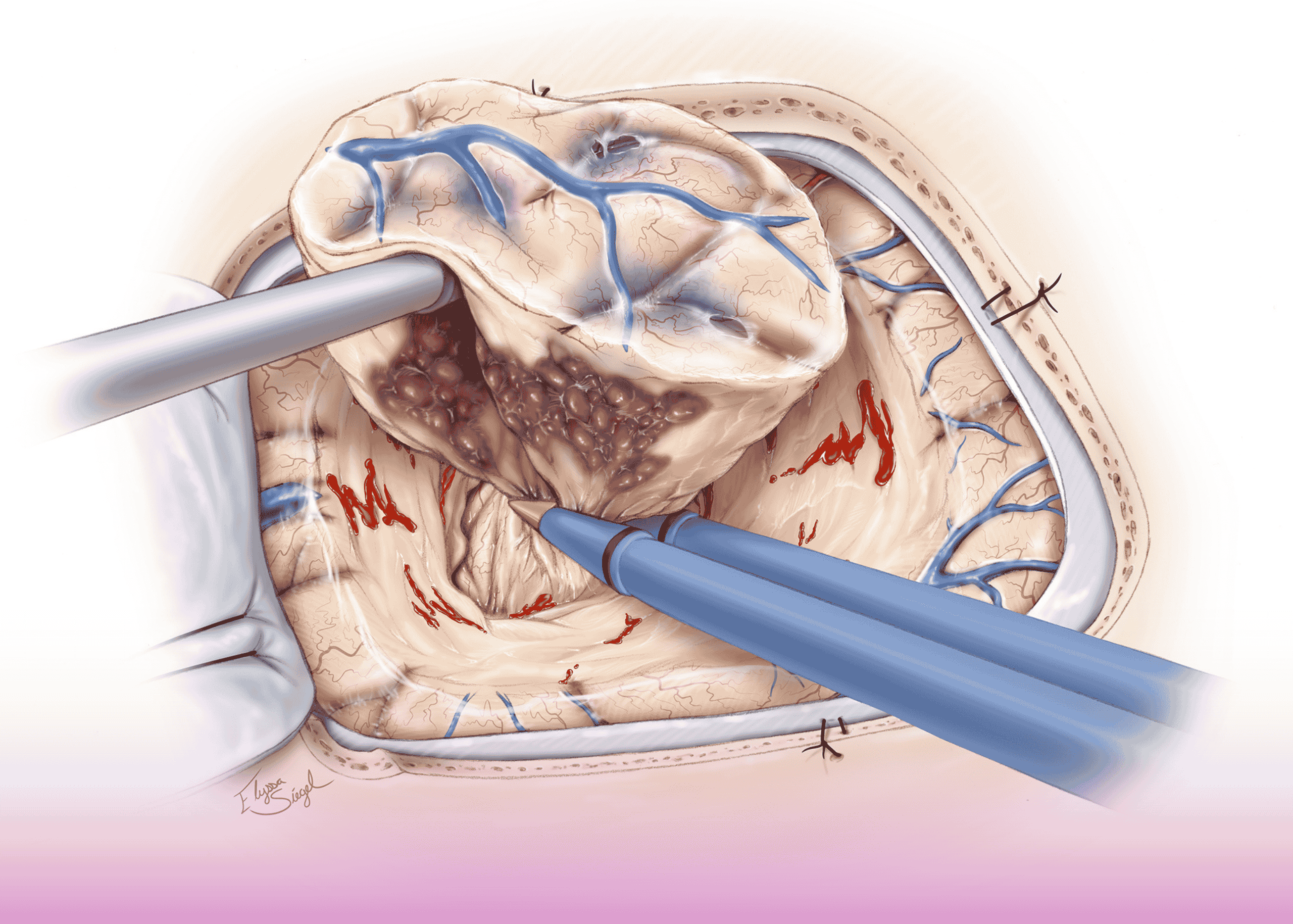
The surgical team performed:
- Mitral valve replacement using a 31 mm Carbomedics mechanical valve
- Excision of vegetation from the aortic valve
- Repair of the aortic valve, where small vegetation was identified on the non-coronary cusps
Surgical Team
The landmark procedure was performed by an expert team comprising:
- Dr. Dinesh Sadasival, Consultant Cardiothoracic Surgeon
- Dr. Tarig Ali, HOD, Cardiothoracic Surgeon
- Dr. Y. A. Nazer, Consultant Cardiac Surgery
- Dr. Arun Vijaykumar, Cardiac Anesthesia
- Dr. Sival Pillai, HOD, Cardiac Anesthesia
Discussion
This case highlights several important clinical considerations in the management of infective endocarditis complicated by septic shock:
Diagnostic Challenges
Infective endocarditis can present with varied and nonspecific symptoms, making early diagnosis challenging. In this case, the patient had experienced prolonged fever for three months before presenting in extremis with respiratory distress. This underscores the importance of considering endocarditis in patients with:
- Unexplained, persistent fever
- Significant weight loss
- New cardiac murmurs
- Predisposing factors such as rheumatic heart disease
Timing of Surgical Intervention
The timing of surgical intervention in infective endocarditis requires careful consideration. Key factors include:
- Hemodynamic stability: In this case, initial stabilization with medical therapy was necessary before proceeding to surgery.
- Control of infection: The two-week course of antibiotics resulting in normalization of inflammatory markers indicated adequate control of the acute infection.
- Prevention of complications: Surgery was planned to prevent further complications such as embolization of vegetation, progressive valve destruction, and persistent heart failure.
Choice of Prosthetic Valve
The decision to use a mechanical valve (31 mm Carbomedics) in this 42-year-old patient aligns with current guidelines that often favor mechanical valves in younger patients who can tolerate long-term anticoagulation. Factors influencing this decision typically include:
- Patient age
- Anticoagulation compliance
- Risk of reinfection
- Hemodynamic performance of the valve
Management of Multi-Valve Involvement
This case also demonstrates the surgical approach to multi-valve involvement in endocarditis. While the mitral valve required replacement due to severe damage, the aortic valve had only small vegetation on the non-coronary cusps, allowing for successful repair rather than replacement. This valve-sparing approach offers several advantages:
- Avoids the need for a second prosthetic valve
- Reduces the risk of prosthetic valve endocarditis
- Preserves native valve hemodynamics
- Potentially reduces the intensity of required anticoagulation
Clinical Significance
This case holds particular significance as the first cardiac surgery performed at Burjeel Specialty Hospital, Sharjah. It demonstrates:
- Successful multidisciplinary collaboration between emergency medicine, infectious disease, cardiology, and cardiac surgery.
- Effective management of a life-threatening condition through appropriate medical stabilization followed by definitive surgical intervention.
- Expansion of advanced cardiac surgical capabilities to Burjeel Specialty Hospital, Sharjah, enhancing access to specialized cardiac care in the region.
Conclusion
This landmark case of successful management of septic shock and infective endocarditis demonstrates the importance of prompt diagnosis, appropriate antimicrobial therapy, and timely surgical intervention. The successful outcome underscores the value of a multidisciplinary approach to complex cardiac conditions and highlights the expanding capabilities of cardiac surgical centers in the region.
The case serves as an important reminder of the need for high clinical suspicion for infective endocarditis in patients with prolonged fever and weight loss, particularly in those with underlying structural heart disease. Early diagnosis and appropriate management remain critical in reducing morbidity and mortality in this challenging clinical entity.