When a 74-year-old man with multiple serious health conditions was diagnosed with aggressive esophageal cancer, many might have considered his case too risky for major surgery. However, the expert team at Burjeel Medical City proved that age and comorbidities don’t have to be barriers to life-saving treatment when advanced robotic surgery techniques are employed.
A Complex Cancer Diagnosis in a High-Risk Patient
The patient’s journey began with chest discomfort in his home country. What started as routine medical evaluation quickly revealed a serious diagnosis that would challenge even the most experienced oncological teams.
Initial Discovery
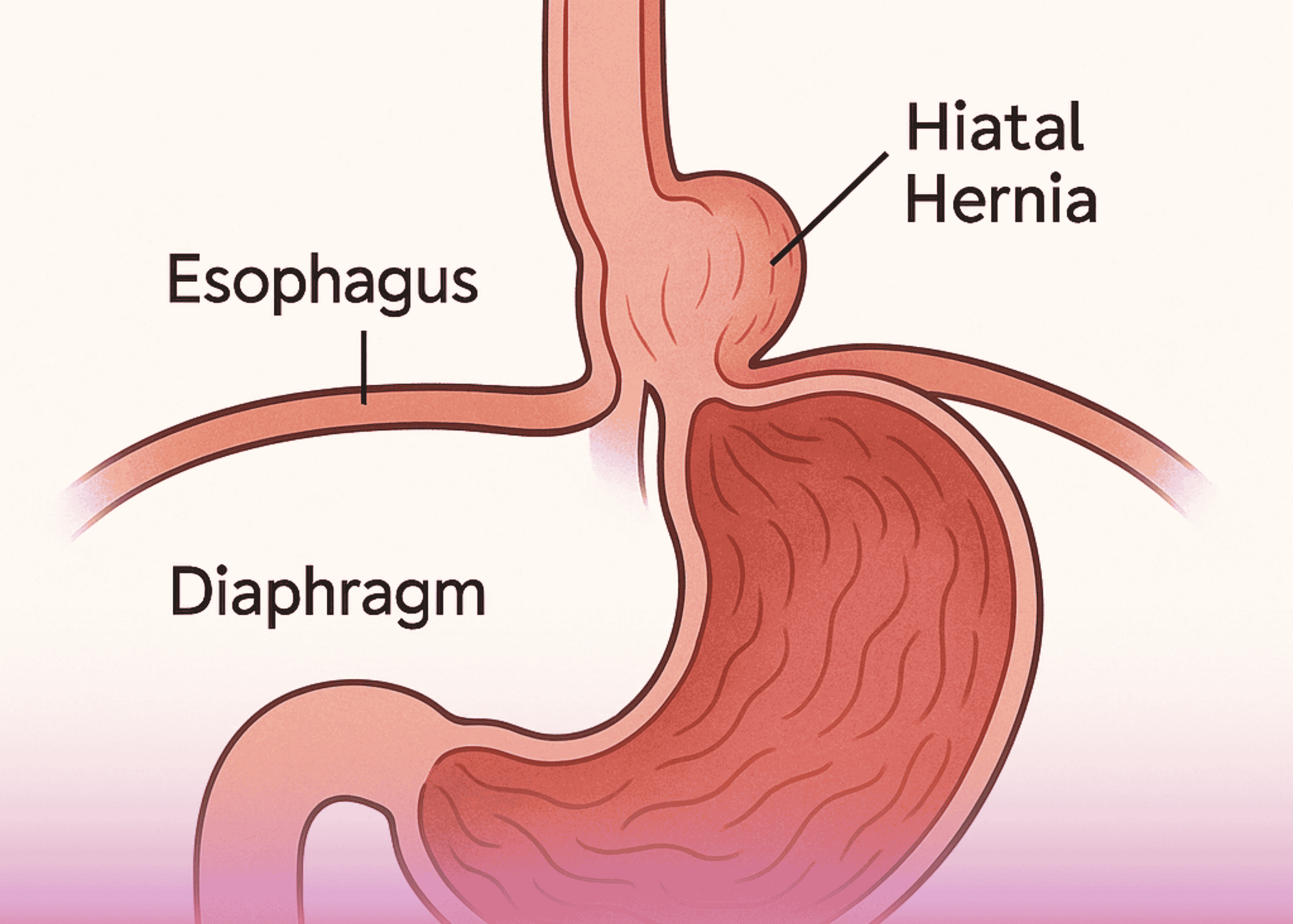
Routine endoscopy revealed concerning findings:
- Mucosal lesion in the mid to lower esophagus
- Hiatus hernia with Barrett’s esophagus
- Histopathology results showing poorly differentiated signet ring cell adenocarcinoma
Signet ring cell adenocarcinoma is particularly aggressive, known for its poor prognosis and challenging treatment requirements, especially in elderly patients.
The Challenge of Multiple Comorbidities
What made this case extraordinarily complex was the patient’s extensive medical history:
- Previous coronary artery bypass grafting (CABG)
- Moderate aortic stenosis
- Hypertension and Type 2 diabetes
- Chronic kidney disease
- Hyperlipidemia
- Interstitial lung disease
This combination of conditions would typically make a patient unsuitable for major surgery, particularly the extensive procedure required for esophageal cancer treatment.
Advanced Staging and Treatment Planning
Upon arrival in the UAE for specialized care, comprehensive staging was performed:
Imaging Studies
- CT scan revealed eccentric wall thickening of the mid-esophagus
- PET scan showed lymph nodes in paratracheal, subcarinal, and paraesophageal regions
- EBUS biopsy of suspicious lymph nodes was negative for malignancy
Multidisciplinary Team (MDT) Approach
The case was presented to Burjeel’s specialized oncology MDT, which includes:
- Gastrointestinal surgeons
- Medical oncologists
- Radiation oncologists
- Anesthesiologists
- Pathologists
The team’s consensus was to proceed with neoadjuvant FLOT chemotherapy followed by surgical re-evaluation.
Neoadjuvant Chemotherapy: Preparing for Surgery
FLOT Chemotherapy Protocol
The patient received four courses of FLOT chemotherapy, a specialized regimen that includes:
- 5-Fluorouracil
- Leucovorin
- Oxaliplatin
- Docetaxel
This intensive treatment aims to:
- Shrink the primary tumor
- Eliminate microscopic disease
- Improve surgical outcomes
- Reduce risk of recurrence
Response Evaluation
After completing chemotherapy, comprehensive re-staging showed no disease progression, making the patient an excellent candidate for surgical intervention despite his high-risk profile.
Revolutionary Robotic Surgery: RAMIE Technique
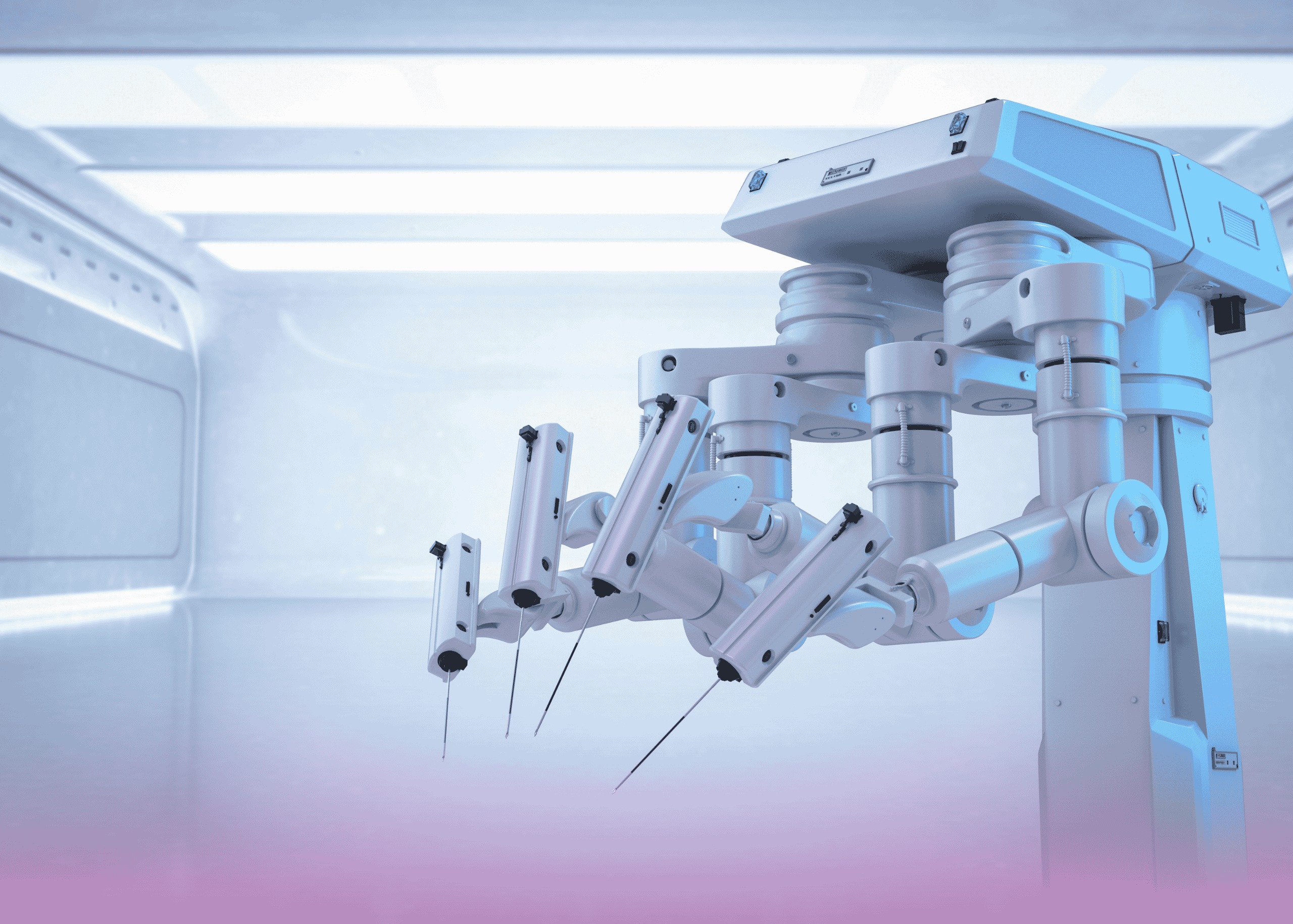
Dr. Ali Iyoob Valiyaveettil, Consultant and Head of Gastrointestinal Surgery, led the team in performing Robot-Assisted Minimally Invasive Esophagectomy (RAMIE) – a cutting-edge technique that represents the future of esophageal cancer surgery.
Why Robotic Surgery for High-Risk Patients?
Traditional open esophagectomy is one of the most challenging surgeries in oncology, with significant risks including:
- Major blood loss
- Extended recovery times
- High complication rates
- Prolonged hospital stays
RAMIE offers revolutionary advantages:
- Minimally invasive approach reduces surgical trauma
- Enhanced precision with robotic arms
- 3D high-definition visualization
- Improved maneuverability in confined spaces
- Reduced post-operative pain
- Faster recovery times
The Complex Three-Stage Procedure
The surgery involved multiple phases, each requiring exceptional surgical skill:
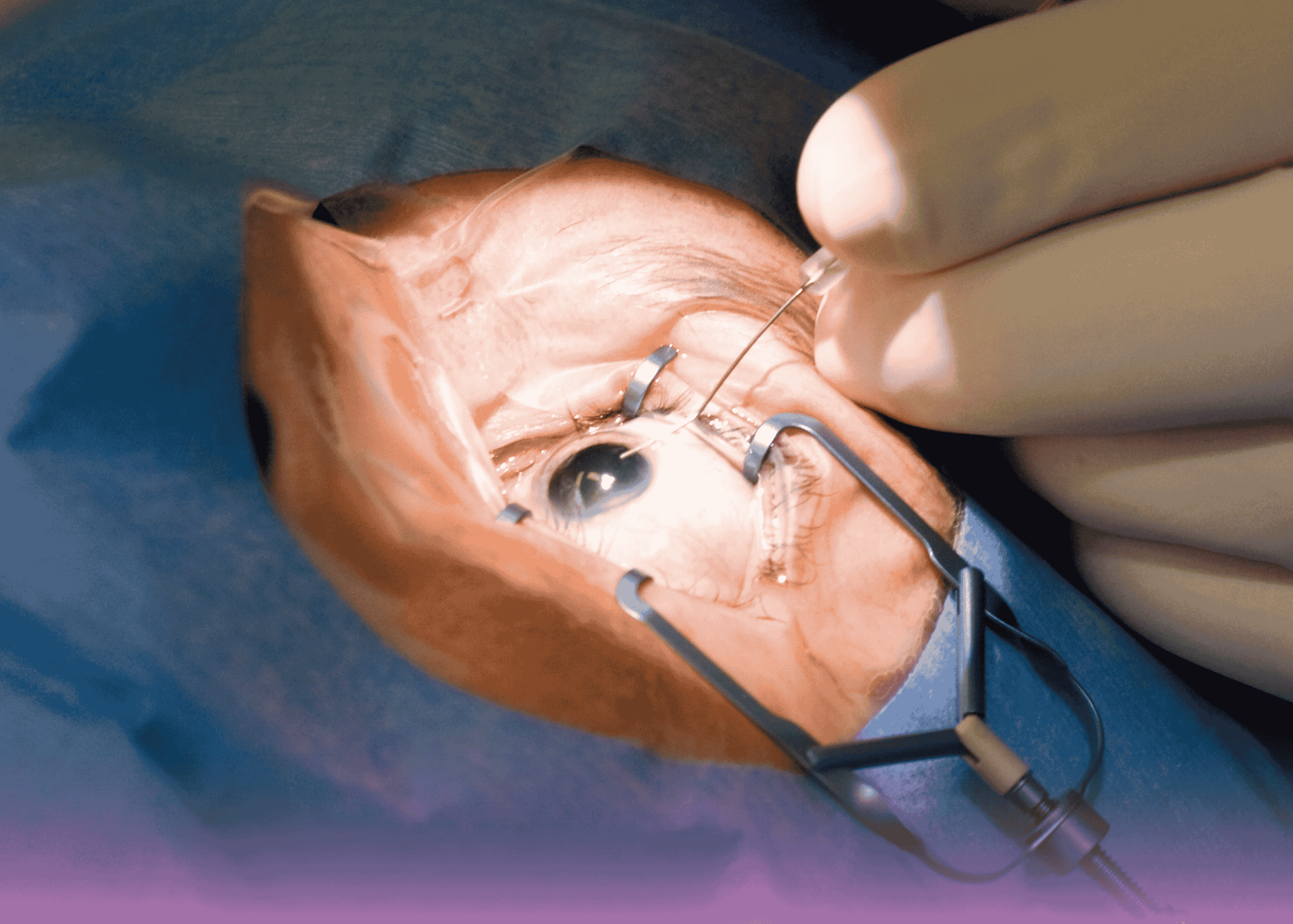
Stage 1: Thoracoscopic Phase
- Patient positioned prone for optimal access
- Radical esophagectomy with complete tumor removal
- Comprehensive lymph node dissection of mediastinal nodes
- Preservation of vital structures
Stage 2: Abdominal Phase
- Gastric conduit preparation using the stomach to replace the esophagus
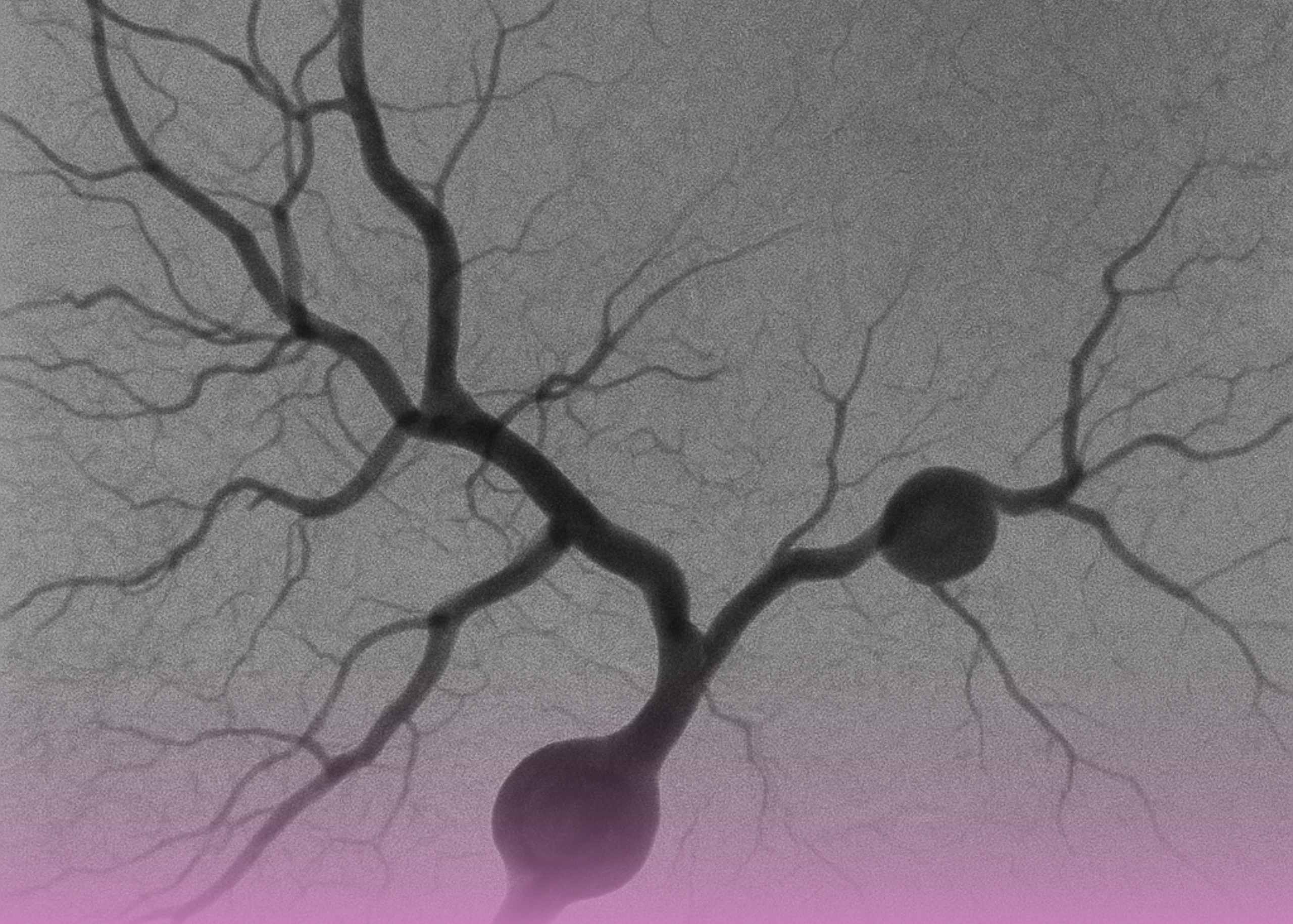
- ICG (Indocyanine Green) test to assess blood supply adequacy
- Pyloroplasty to improve gastric emptying
- Careful preservation of gastric blood vessels
Stage 3: Cervical Phase
- Neck incision for anastomosis creation
- Side-to-side connection between gastric conduit and remaining esophagus
- Meticulous technique to prevent leakage
- No feeding tubes required due to superior surgical technique
Advanced Intraoperative Technology
The procedure utilized state-of-the-art technology:
Da Vinci Xi Robotic System
- Four robotic arms with enhanced dexterity
- 3D high-definition visualization
- Tremor elimination for precise movements
- Scaled motion for fine tissue manipulation
ICG Fluorescence Imaging
- Real-time assessment of tissue blood supply
- Prevention of anastomotic complications
- Immediate visualization of perfusion quality
Expert Surgical Team Excellence
The successful outcome was achieved through the collaboration of:
Remarkable Recovery and Outcomes
Despite the patient’s high-risk profile, the results exceeded expectations:
Immediate Post-Operative Period
- ICU monitoring for 2 days as precaution
- Nasogastric tube removal after 48 hours
- Contrast swallow study showing normal passage with no leaks
- Early mobilization reducing complications
Rapid Recovery Milestones
- Oral feeding started within 48 hours
- Progression to puree diet without problems
- Chest tube removal after 72 hours
- Abdominal drain removal after 72 hours
- No voice changes or breathing difficulties
- Clean wound healing
Hospital Discharge
The patient was discharged on the 7th post-operative day – remarkably fast for such extensive surgery, especially in an elderly patient with multiple comorbidities.
Pathology Results and Long-Term Prognosis
Histopathology Findings
- Poorly differentiated adenocarcinoma (Grade 3)
- ypT3N1 staging (1 out of 26 lymph nodes positive)
- Good response to neoadjuvant chemotherapy
- Clear surgical margins
Unexpected Finding
Multiple lymph nodes showed caseating granulomatous changes, indicating possible concurrent inflammatory conditions that were successfully managed.
The Advantages of Minimally Invasive Esophagectomy
This case demonstrates why RAMIE is becoming the gold standard for esophageal cancer surgery:
Reduced Morbidity
- Lower complication rates compared to open surgery
- Decreased blood loss during the procedure
- Reduced post-operative pain
- Faster return to normal activities
Superior Oncological Outcomes
- Better lymph node clearance due to enhanced visualization
- Reduced positive margin rates
- Improved long-term survival in many studies
Enhanced Recovery
- Shorter ICU stays reduce healthcare costs
- Earlier hospital discharge improves patient satisfaction
- Faster return to baseline function
Overcoming the Learning Curve Challenge
One of the traditional barriers to minimally invasive esophagectomy has been the steep learning curve for surgeons. However, robotic assistance helps overcome this challenge:
Robotic Advantages for Surgeons
- Intuitive movements that mirror hand motions
- Enhanced dexterity in confined spaces
- Tremor elimination for precise dissection
- 3D visualization improves depth perception
Training and Expertise
Burjeel Medical City’s commitment to surgical excellence includes:
- Specialized training programs for robotic surgery
- Continuous education in latest techniques
- Volume requirements ensuring surgeon proficiency
- Multidisciplinary collaboration
Why Choose Burjeel for Complex Cancer Surgery?
This successful case highlights several key advantages:
Advanced Technology
- Latest Da Vinci Xi robotic system
- Integrated OR technology for seamless procedures
- Real-time imaging capabilities
- Comprehensive monitoring systems
Specialized Expertise
- High-volume esophageal surgery program
- Experienced robotic surgeons
- Multidisciplinary cancer care team
- Specialized anesthesia for complex cases
Comprehensive Care
- Neoadjuvant and adjuvant therapy coordination
- Nutritional support services
- Rehabilitation programs
- Long-term follow-up care
The Future of Esophageal Cancer Treatment
This case represents the evolution toward personalized, minimally invasive cancer care:
Precision Medicine
- Molecular profiling of tumors for targeted therapy
- Personalized treatment protocols based on patient factors
- Biomarker-guided therapy selection
Technological Advances
- Enhanced robotic systems with improved capabilities
- Artificial intelligence integration for surgical planning
- Advanced imaging for better staging and monitoring
Patient Selection: Making High-Risk Surgery Safer
This case demonstrates that with proper evaluation and advanced techniques, many patients previously considered unsuitable for surgery can achieve excellent outcomes:
Comprehensive Pre-Operative Assessment
- Cardiac evaluation and optimization
- Pulmonary function testing
- Nutritional assessment and support
- Multidisciplinary consultation
Risk Mitigation Strategies
- Enhanced recovery protocols
- Specialized anesthesia techniques
- Minimally invasive approaches
- Expert post-operative care
Conclusion: Hope for Complex Cancer Patients
The successful treatment of this 74-year-old patient with multiple comorbidities demonstrates that:
- Age alone should not exclude patients from curative surgery
- Robotic technology can make complex procedures safer
- Multidisciplinary care improves outcomes significantly
- Expert surgical teams can achieve excellent results in challenging cases
- Advanced techniques continue to expand treatment options
For patients and families facing similar diagnoses, this case provides hope that even complex situations can be successfully managed with the right expertise, technology, and comprehensive care approach.
The future of esophageal cancer treatment lies in this combination of advanced technology, surgical expertise, and personalized care – exactly what Burjeel Medical City provides to every patient.