Introduction
Skull base tumors represent some of the most challenging conditions in neurosurgery. Their deep location, proximity to vital neurovascular structures, and complex surrounding anatomy make them particularly difficult to access and remove safely. Among these rare entities, clival chordomas stand out as especially challenging lesions that require multidisciplinary expertise and advanced technological approaches.
This case study explores the successful management of a clival chordoma in a young patient at Burjeel Medical City (BMC), highlighting the integration of cutting-edge minimally invasive techniques, intraoperative imaging, and comprehensive multidisciplinary care that resulted in an optimal outcome for a potentially devastating condition.
Understanding Clival Chordomas
What are Chordomas?
Chordomas are rare, slow-growing malignant tumors that develop from remnants of the notochord, an embryonic structure involved in the development of the spine. These tumors typically arise along the axial skeleton, with approximately 35% occurring at the skull base (clivus), 50% at the sacrum, and 15% in the mobile spine.
With an incidence of approximately 8 cases per 10 million people, clival chordomas are exceedingly rare. They typically present in adults between 40-60 years of age, though they can occur in any age group.
Clinical Presentation
The clinical manifestation of clival chordomas depends on their size, exact location, and the surrounding structures they compress or invade. Common presentations include:
- Cranial nerve deficits: Due to compression of cranial nerves traversing the skull base
- Headaches: Often due to increased intracranial pressure or direct pressure on pain-sensitive structures
- Visual disturbances: Including double vision (diplopia), visual field defects, or decreased visual acuity
- Brainstem compression symptoms: May include balance problems, motor or sensory deficits
- Pituitary dysfunction: If the tumor extends into the sellar region
Diagnostic Challenges
Diagnosing clival chordomas presents several challenges:
- Rarity: Many clinicians may never encounter a case during their entire career
- Nonspecific symptoms: Initial symptoms like headache or double vision may be attributed to more common conditions
- Deep location: The tumor’s position at the skull base makes clinical examination difficult
- Variable radiographic appearance: Can mimic other skull base lesions
Case Presentation
Patient Profile
The patient in this case was a 35-year-old Pakistani gentleman who worked as a driver. His presenting complaint was double vision (diplopia) that had developed over a period of a few months, progressively worsening to the point where it significantly interfered with his daily activities and forced him to stop driving.
The patient initially sought medical attention at another hospital, where he was found to have paralysis of the left sixth cranial nerve (abducens nerve), which controls lateral eye movement. This explained his diplopia, as the abducens nerve palsy resulted in impaired ability to abduct the left eye.
Diagnostic Workup
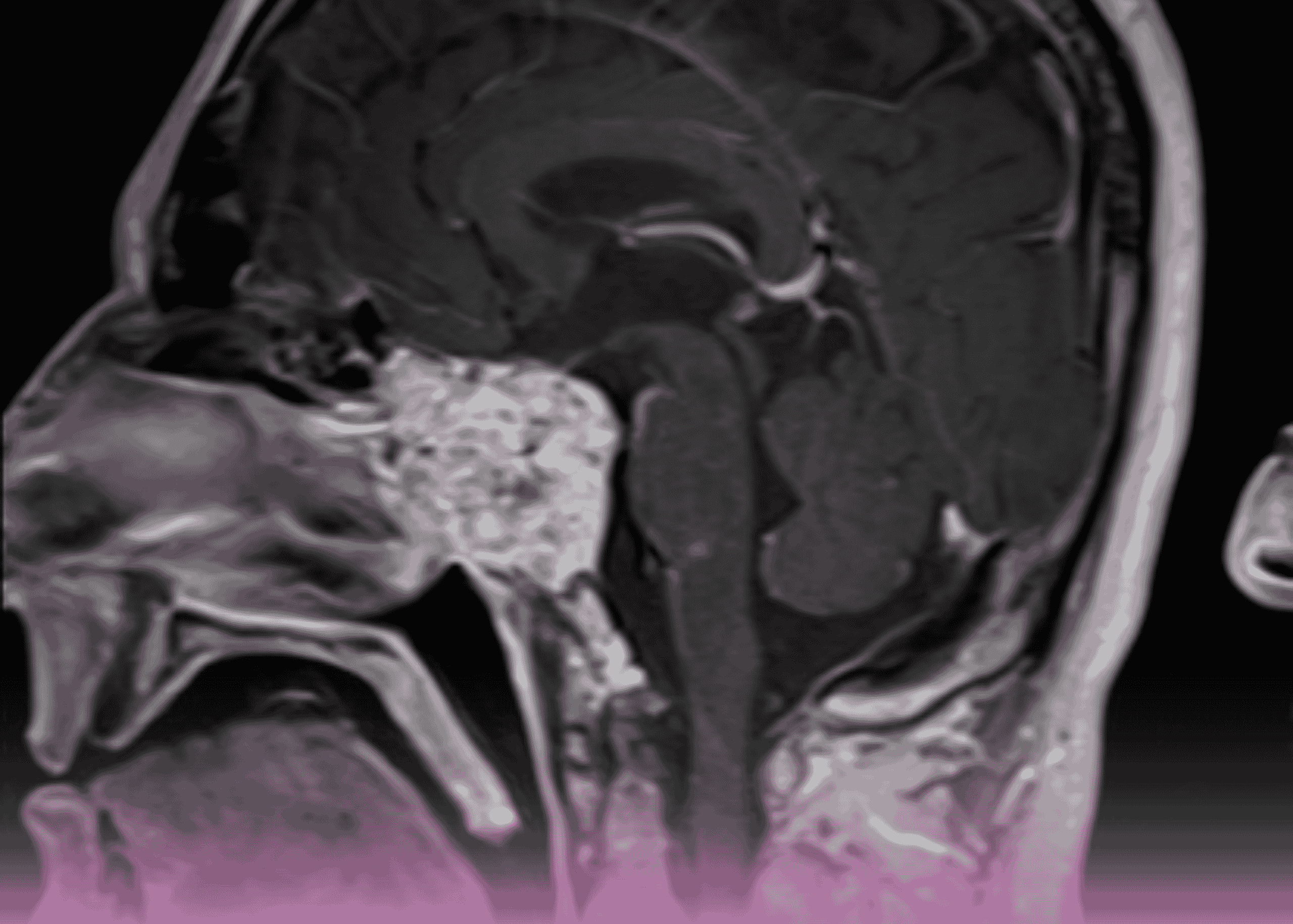
The patient underwent magnetic resonance imaging (MRI) which revealed a concerning finding: an extra-axial abnormal signal intensity area in the prepontine cistern along the clivus. The lesion measured approximately 33 × 16 × 29 mm in craniocaudal, anteroposterior, and transverse dimensions.
The imaging characteristics included:
- Low signal intensity on T1-weighted images
- Heterogeneous signal on T2-weighted and FLAIR images
- Heterogeneous signal on diffusion-weighted imaging
- No significant enhancement on post-contrast images
The lesion demonstrated an infiltrative nature, invading and compressing the pons with a clear mass effect on the brainstem. Additionally, the vertebral artery was displaced toward the left. The tumor partially extended into the sella, compressing the pituitary gland, and laterally abutted the left temporal lobe and bilateral cavernous sinuses, with possible extension into the left cavernous sinus.
These radiological findings were highly suggestive of a clival chordoma, a rare skull base tumor.
Initial Diagnosis
Based on the clinical presentation and imaging findings, an initial diagnosis of a retroclival large mass with brain stem compression was made, with clival chordoma being the most likely etiology.
Comprehensive Treatment Approach
Multidisciplinary Assessment
Upon referral to Burjeel Medical City, the patient underwent a thorough evaluation in the neurosurgery clinic. The neurosurgical team explained his condition in detail and discussed various treatment options.
Additional investigations were conducted, including:
- Endocrine workup: To assess any impact on pituitary function
- Formal visual assessment: To document the extent of visual impairment
The case was then presented at the Oncology Tumor Board, headed by Prof. Humaid Obaid bin Harmal Al Shamsi, with participation from specialists in radiology, medical oncology, and radiation oncology. Following comprehensive discussion, the board recommended surgical intervention as the primary treatment modality, with subsequent adjuvant therapy to be determined based on histopathological findings.
Surgical Planning
The surgical team opted for a minimally invasive endoscopic endonasal trans-clival approach. This modern technique avoids the need for craniotomy and brain retraction by accessing the tumor through the natural corridor of the nasal cavity and sinuses. The surgical plan included:
- Endoscopic Trans-Nasal Trans-Clival Microsurgical Resection: A minimally invasive approach to access and remove the tumor
- Neuronavigation Guidance: Advanced computer-assisted technology to provide real-time surgical orientation
- Electrophysiological Monitoring: Continuous monitoring of neural function during surgery to minimize the risk of neurological injury
- Intraoperative Frozen Section: To confirm the diagnosis during surgery
- Skull Base Reconstruction: To repair the surgical defect and prevent postoperative cerebrospinal fluid leak
Surgical Execution
The surgery proceeded as planned, with an endoscopic approach through the nasal cavity. During the procedure, several key steps were executed:
- A biopsy with intraoperative frozen section analysis confirmed the diagnosis of clival chordoma
- The surgical team performed a meticulous resection of the tumor through a narrow corridor between critical neurovascular structures
- While the patient was still under anesthesia, an intraoperative MRI was performed, revealing a small residual portion of the tumor hidden behind the left carotid artery
- Based on this crucial information, the patient was immediately returned to surgery for further resection to achieve gross total removal of the tumor
This case highlights the significant value of intraoperative MRI technology, which allowed the surgeons to identify residual tumor that might otherwise have been missed, enabling a more complete resection in a single surgical session.
A follow-up MRI performed 24 hours after surgery confirmed gross total resection of the tumor with no visible residual.
Multidisciplinary Post-Surgical Management
Following the final histopathological confirmation of clival chordoma, the case was again presented to the Tumor Board for discussion of adjuvant therapy. Based on the tumor characteristics and extent of resection, adjuvant radiotherapy was recommended to reduce the risk of recurrence.
This comprehensive, multi-stage approach to treatment planning exemplifies the value of multidisciplinary collaboration in managing complex oncological cases.
Challenges and Considerations
The management of this case involved several significant challenges:
1. Rarity of the Condition
With an estimated incidence of only 8 cases per 10 million people, clival chordomas are exceptionally rare. Consequently, few neurosurgeons gain substantial experience in managing these tumors, making each case a significant technical challenge requiring specialized expertise.
2. Critical Anatomical Location
The tumor’s position at the skull base presented formidable anatomical challenges:
- Located behind the clival bone and anterior to the brainstem
- Difficult to access transcranially without significant risk of neurological morbidity
- Situated in close proximity to critical vascular structures, including the carotid arteries anteriorly and the basilar artery posteriorly
- Adjacent to multiple cranial nerves that could be damaged during surgery
3. Technical Surgical Challenges
The endoscopic approach, while minimally invasive, presented its own technical demands:
- Operating through a narrow corridor with limited maneuverability
- Navigating between vital structures with minimal margin for error
- Working with a 4mm endoscope through the nasal passage to access a deep-seated tumor
- Creating a surgical window through the clival bone between the carotid arteries (approximately 1cm wide by 1.5cm high) to remove a 3cm tumor
4. Oncological Considerations
Chordomas present unique oncological challenges:
- Currently, the median survival for patients with clival chordomas is approximately 7 years
- The overall survival rates are reported as 68% at 5 years and 40% at 10 years
- Complete surgical resection offers the best chance for long-term survival, potentially reaching 67% at 10 years
- The tumor’s proximity to critical structures often makes complete resection difficult to achieve safely
Technological Advantages
This case demonstrates the impact of advanced technology in modern neurosurgery:
Endoscopic Skull Base Surgery
Endoscopic approaches represent the cutting edge of skull base surgery, offering:
- Minimally invasive access through natural corridors
- Excellent visualization with magnified, high-definition views
- Reduced collateral damage to surrounding structures
- Faster recovery compared to traditional open approaches
Intraoperative MRI
The availability of intraoperative MRI proved crucial in this case:
- Identified residual tumor that would otherwise have been missed
- Enabled immediate return to surgery for complete resection
- Eliminated the need for a second operation
- Potentially improved long-term oncological outcomes
Comprehensive Cancer Center Capabilities
Burjeel Cancer Institute at BMC offered several advantages:
- A highly trained, subspecialized team of physicians
- State-of-the-art equipment and facilities
- Up-to-date treatment protocols
- Complete continuum of care from diagnosis through surgery and adjuvant therapy
Conclusion
This case illustrates the successful management of a rare and challenging clival chordoma through a state-of-the-art minimally invasive approach. The integration of advanced surgical techniques, intraoperative imaging, and multidisciplinary collaboration exemplifies modern neuro-oncological care at its best.
The comprehensive capabilities at Burjeel Medical City—including specialized surgical expertise, advanced intraoperative imaging, and multidisciplinary tumor board—were instrumental in achieving an optimal outcome in this case. For rare and complex conditions like clival chordomas, such a comprehensive approach offers patients the best opportunity for successful treatment and improved quality of life.
This case serves as an excellent example of how technological advancement and multidisciplinary collaboration can overcome even the most challenging neurosurgical conditions, providing hope and healing for patients facing rare and difficult-to-treat disorders.