Understanding a Rare Skull Base Tumor
Clival chordomas represent one of the most challenging pathologies in neurosurgery. These rare tumors, arising from remnants of the primitive notochord, occur at an incidence of only about 0.8 per 100,000 people, with approximately 35% affecting the spheno-occipital region. Despite their rarity, these tumors demand attention due to their locally aggressive behavior and tendency to compress critical neural structures, particularly the brainstem. A recent case at Burjeel Medical City highlights the sophisticated surgical approaches now available for these complex lesions.
The Clinical Presentation: From Subtle Signs to Serious Symptoms
The patient in this case presented with a constellation of progressive neurological symptoms that had developed over several months, including:
- Persistent headaches that gradually increased in severity
- Visual disturbances including diplopia (double vision)
- Progressive weakness and coordination problems
- Difficulty with swallowing and speech articulation
What made this case particularly concerning was the evidence of significant brainstem compression on imaging studies. The brainstem houses vital neural pathways and control centers for essential functions such as breathing, heart rate regulation, and consciousness. Any compression of this critical structure represents a life-threatening condition requiring urgent intervention.
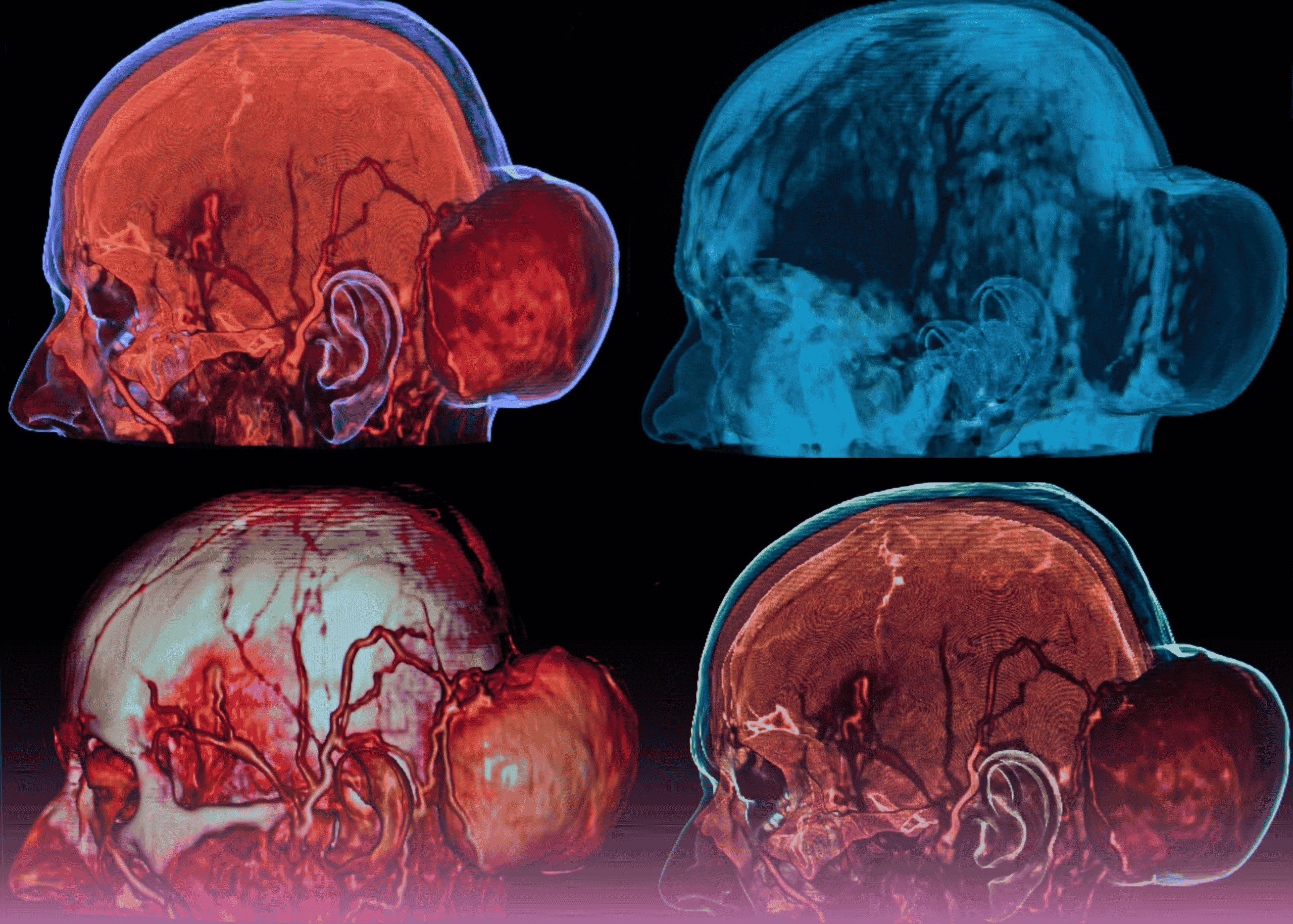
Advanced Imaging: Revealing the Full Extent of the Challenge
The diagnostic workup for this patient included state-of-the-art neuroimaging that revealed the true complexity of the case:
- MRI demonstrated a large, heterogeneously enhancing mass centered in the clivus
- The tumor showed characteristic “honeycomb” appearance typical of chordomas
- Critical findings included significant ventral compression of the brainstem
- Evidence of T2 signal changes within the brainstem suggested early signs of damage from compression
- CT imaging revealed extensive bony erosion of the skull base
The proximity to vital neurovascular structures, including the basilar artery and multiple cranial nerves, further complicated the surgical planning. This constellation of findings characterized a skull base chordoma with significant brainstem compression—a scenario that represents one of the most technically demanding challenges in neurosurgery.
Multidisciplinary Treatment Planning: The Foundation of Success
The management of this complex case began with comprehensive multidisciplinary discussion, bringing together:
- Neurosurgeons specializing in skull base approaches
- Otolaryngologists with expertise in endoscopic techniques
- Neuroradiologists for detailed imaging interpretation
- Radiation oncologists for adjuvant treatment planning
- Neuro-anesthesiologists for complex airway management
This collaborative approach allowed for careful consideration of all treatment options, weighing the risks and benefits of various surgical corridors and techniques. The primary goal was maximal safe resection of the tumor to decompress the brainstem, while preserving neurological function and establishing a clear diagnosis for subsequent targeted therapy.
Surgical Approach: Endoscopic Endonasal Transclival Technique
After careful deliberation, the surgical team selected an endoscopic endonasal transclival approach for this challenging lesion. This minimally invasive technique offers several advantages:
- Direct midline access to the clivus and ventral brainstem
- Avoidance of brain retraction that would be required with transcranial approaches
- Excellent visualization of the tumor and critical neurovascular structures
- Reduced manipulation of cranial nerves
- Lower morbidity compared to traditional open approaches
The procedure involved collaboration between neurosurgery and otolaryngology teams, with specialized instrumentation including high-definition endoscopy, neuronavigation, and intraoperative neurophysiological monitoring to ensure maximal safety during this delicate operation.
Technical Highlights of the Procedure
The surgical approach consisted of several critical phases:
- Nasal Phase: Creation of bilateral nasoseptal flaps for subsequent reconstruction, followed by creation of a wide sphenoidotomy and posterior ethmoidectomy
- Sphenoid Phase: Removal of the sphenoid rostrum and posterior nasal septum to create a wide surgical corridor
- Clival Phase: Removal of the clival bone using high-speed drills and ultrasonic bone cutters to expose the dura
- Dural and Tumor Phase: Careful opening of the dura and systematic removal of tumor tissue with meticulous attention to the preservation of vital structures
- Brainstem Decompression: Gentle dissection of tumor from the ventral surface of the brainstem, with continuous neurophysiological monitoring
- Reconstruction Phase: Multilayered closure using the previously harvested nasoseptal flap to prevent postoperative cerebrospinal fluid leakage
Throughout the procedure, the surgical team maintained constant vigilance regarding brainstem function through neurophysiological monitoring, and preserved critical vascular structures including the basilar artery and its perforator branches.
Postoperative Course and Outcomes
Following surgery, the patient was monitored in the neurosurgical intensive care unit with particular attention to:
- Neurological status, with serial examinations to detect any new deficits
- Airway patency and respiratory function
- Fluid and electrolyte balance, with close monitoring for diabetes insipidus
- Signs of potential cerebrospinal fluid leakage
Postoperative imaging confirmed excellent tumor resection and, more importantly, successful decompression of the brainstem. The patient experienced progressive improvement in preoperative symptoms, with resolution of headaches, improvement in visual symptoms, and gradual recovery of strength and coordination.
Following a period of intensive rehabilitation, the patient was able to return to independent functioning, representing a remarkable outcome for a condition that historically carried high morbidity and mortality rates.
Adjuvant Therapy: Completing the Treatment Paradigm
Given the high recurrence rates associated with chordomas, even after apparently complete surgical resection, the treatment plan included adjuvant therapy. The patient underwent:
- High-precision proton beam therapy, which allows for delivery of high radiation doses to the tumor bed while minimizing exposure to adjacent critical neural structures
- Regular imaging surveillance to detect any early signs of recurrence
- Continued multidisciplinary follow-up to monitor for late complications
Learning Points and Clinical Significance
This challenging case highlights several important principles in contemporary neurosurgery:
- Early diagnosis is critical: Progressive neurological symptoms, particularly when associated with evidence of brainstem compression, require urgent evaluation and intervention.
- The value of minimally invasive approaches: Endoscopic techniques have revolutionized the treatment of skull base lesions, allowing for effective tumor resection with reduced morbidity.
- Multidisciplinary collaboration: The complexity of skull base tumors demands the integration of multiple specialties for optimal outcomes.
- The importance of specialized technology: Advanced neuroimaging, neuronavigation, endoscopy, and neurophysiological monitoring are essential components of safe and effective skull base surgery.
- Comprehensive care beyond surgery: Complete management of chordomas requires integration of adjuvant therapies and long-term surveillance.
Conclusion: A Testament to Modern Neurosurgical Capabilities
The successful management of this challenging clival chordoma with brainstem compression at Burjeel Medical City demonstrates the remarkable advances in contemporary neurosurgery. Through the integration of cutting-edge technology, minimally invasive techniques, and multidisciplinary collaboration, even the most formidable neurosurgical challenges can be addressed with favorable outcomes.
This case serves as an inspiration for patients facing similar diagnoses and reinforces the critical importance of seeking care at centers with specialized expertise in complex skull base surgery.