Introduction
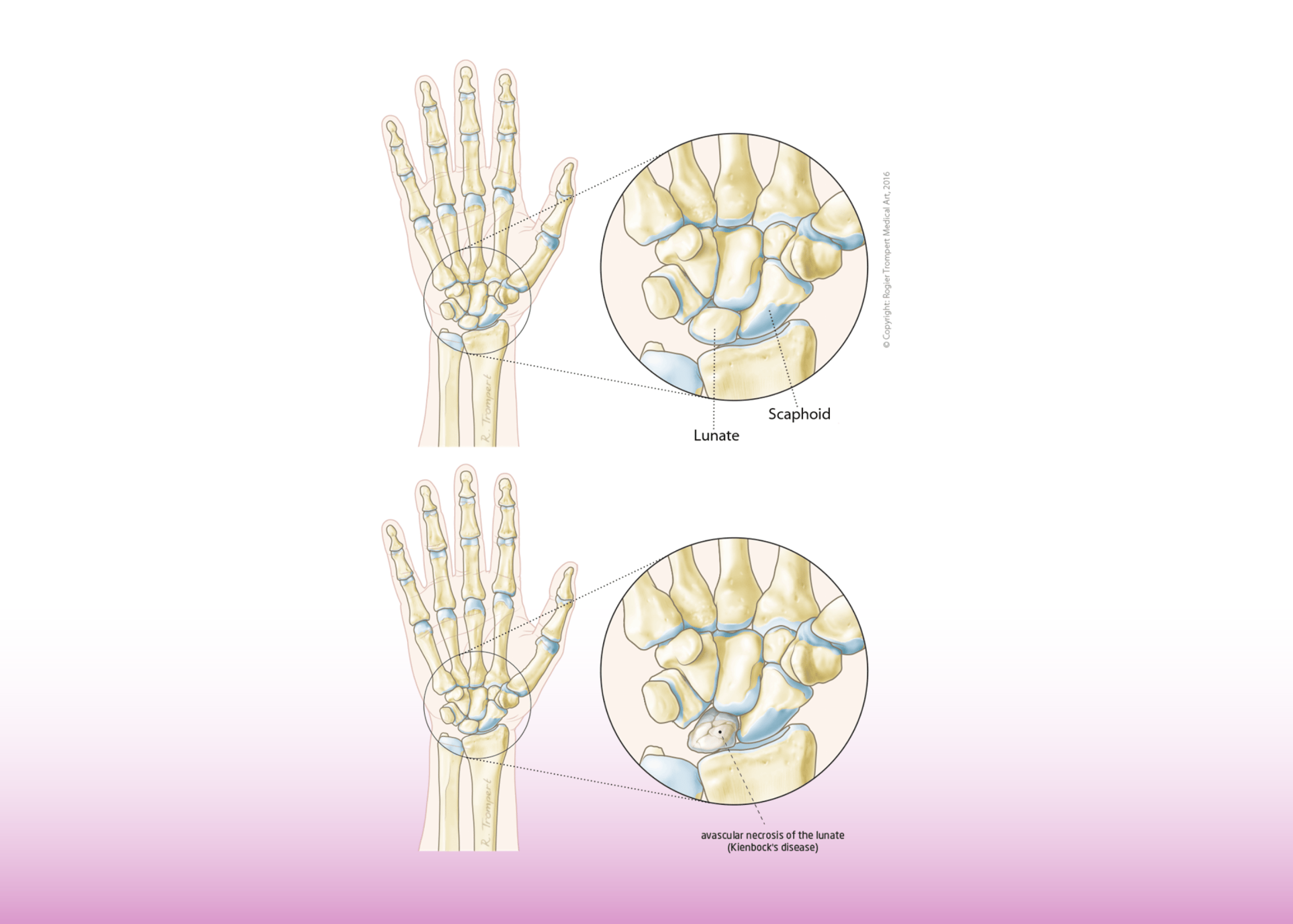
Kienbock’s disease, a relatively rare condition affecting the lunate bone in the wrist, presents significant challenges for both patients and surgeons. This progressive disorder is characterized by avascular necrosis (death of bone tissue due to insufficient blood supply) of the lunate, one of the eight small carpal bones that make up the wrist. Left untreated, the condition leads to wrist pain, diminished grip strength, limited motion, and eventually, debilitating arthritis.
This case study explores an advanced surgical approach – the vascularized bone graft – for managing a case of advanced Kienbock’s disease in a young patient. The procedure, performed at Burjeel Hospital in Abu Dhabi, demonstrates how microsurgical techniques can offer hope for patients with conditions previously considered difficult to treat effectively.
Understanding Kienbock’s Disease
Pathophysiology
Kienbock’s disease involves the progressive collapse of the lunate bone in the wrist due to compromised blood supply. This vascular disruption leads to bone necrosis, fragmentation, and eventual collapse, resulting in altered wrist mechanics, pain, and functional limitations.
The condition typically progresses through several stages:
- Stage I: Ischemia (reduced blood supply) without radiographic changes
- Stage II: Sclerosis (hardening) of the lunate visible on X-rays
- Stage III: Collapse and fragmentation of the lunate
- Stage IIIA: Lunate collapse without scaphoid rotation
- Stage IIIB: Lunate collapse with fixed scaphoid rotation
- Stage IV: Advanced collapse with degenerative changes throughout the wrist
Risk Factors
Several factors may contribute to the development of Kienbock’s disease:
- Anatomical variations: A shorter ulna relative to the radius (negative ulnar variance) may increase mechanical stress on the lunate
- Vascular anatomy: Variations in blood supply to the lunate can predispose to ischemia
- Trauma: History of wrist injury
- Systemic factors: Conditions affecting blood flow or coagulation
- Occupational factors: Activities involving repetitive wrist loading or vibration
Clinical Presentation
Patients with Kienbock’s disease typically present with:
- Wrist pain, particularly during activities
- Swelling and tenderness over the lunate area
- Limited range of motion
- Decreased grip strength
- In advanced stages, wrist instability and crepitus
Case Presentation
Patient Profile
A 31-year-old female presented with persistent pain in her left wrist of approximately one year’s duration. Her medical history included a traumatic injury to the left wrist one year prior, which was conservatively managed at another facility. Despite this management, she continued to experience persistent wrist pain, leading to her referral to Burjeel Hospital with a diagnosis of Kienbock’s disease.
Clinical Findings
On examination, the patient exhibited:
- Diffuse swelling around the left wrist
- Tenderness throughout the wrist, particularly over the lunate area
- Painful and restricted range of motion
Diagnostic Imaging
The radiographic assessment revealed:
- X-rays showing sclerosis of the lunate
- Loss of height of the lunate bone
- Fragmentation of the lunate structure
Magnetic Resonance Imaging (MRI) confirmed these findings and supported the diagnosis of advanced Kienbock’s disease, classified as Stage 3A according to Lichtman’s classification system. At this stage, the lunate had undergone collapse but without scaphoid rotation or carpal instability.
Treatment Approach
Surgical Options Assessment
For Stage 3A Kienbock’s disease, several surgical options exist:
- Proximal Row Carpectomy: Removal of the scaphoid, lunate, and triquetrum bones
- Limited Wrist Fusion: Joining certain carpal bones to redistribute forces
- Revascularization Procedures: Techniques to restore blood supply to the lunate
- Total Wrist Arthrodesis: Complete fusion of the wrist in severe cases
- Denervation Procedures: To reduce pain while maintaining some motion
After thorough discussion with the patient regarding the risks, benefits, and long-term outcomes of each approach, a revascularization procedure was selected. This decision was based on the patient’s young age, the stage of disease, and the desire to preserve wrist function.
Surgical Technique
The patient underwent a specialized procedure performed by the Specialist Orthopedic Surgeon, Dr. Jayakrishnan Narayana Kurup by combining several techniques:
- 4+5 Extensor Compartmental Artery-Based Vascularized Bone Graft: This microsurgical procedure involves harvesting bone with its blood supply from the dorsal distal radius and transferring it to the lunate to provide both structural support and blood supply.
- Posterior Interosseous Nerve (PIN) Neurectomy: Division of a nerve branch to reduce pain signals from the affected area.
- Scapho-capitate Pinning: Temporary stabilization of these carpal bones with Kirschner wires (K-wires) to maintain proper alignment during healing.
Technical Challenges
The surgical team faced several challenges during this procedure:
- Microsurgical Complexity: The harvesting of bone with its minute blood vessel supply requires advanced microsurgical expertise and specialized equipment.
- Anatomical Variations: The 4+5 extensor compartmental artery is small and can have variable anatomy between patients.
- Vascular Pedicle Preservation: Maintaining the viability of the blood vessels during transfer is critical and technically demanding.
- Recipient Site Preparation: Creating an appropriate cavity in the necrotic lunate while preserving its outer shell.
Surgical Implementation
The procedure was performed under general anesthesia with a tourniquet applied to the upper arm. A detailed step-by-step approach was followed:
- A dorsal approach to the wrist was utilized to expose both the 4th and 5th extensor compartments and the lunate.
- The Posterior Interosseous Nerve was identified and neurectomy performed to provide pain relief.
- The lunate was accessed and a cavity created after curettage of the necrotic bone while preserving its outer shell.
- A vascularized bone graft based on the 4+5 extensor compartmental artery was harvested from the distal radius, with careful preservation of its vascular pedicle.
- The vascularized bone graft was transferred and inserted into the prepared cavity in the lunate.
- Temporary scapho-capitate pinning was performed with K-wires to provide stability during the healing process.
- Meticulous closure was performed in layers.
Intraoperative photographs documented key steps of the procedure, including:
- PIN nerve identification before neurectomy
- Preparation of the cavity in the lunate after curettage
- Harvesting of the bone graft with its vascular pedicle
- Insertion of the vascularized bone graft into the lunate cavity
Post-Operative Course
The perioperative period was uneventful, with the patient discharged on the same day following appropriate pain management and wound care instructions. A below-elbow splint was applied to protect the wrist during the initial healing phase.
Post-operative radiographs demonstrated:
- Restoration of lunate height
- Proper positioning of the scapho-capitate K-wires
- Maintained carpal alignment
Clinical Outcome
At the six-month follow-up assessment, the patient reported significant improvement:
- Pain-free wrist
- Ability to perform daily activities without discomfort
- Progressive improvement in range of motion
- Return to normal hand function for most activities
Radiographic evaluation at six months showed signs of lunate revascularization with maintenance of carpal height and alignment.
Discussion
Significance of Vascularized Bone Grafting
Vascularized bone grafting represents an important advancement in the management of Kienbock’s disease, particularly for younger patients in whom preservation of wrist mechanics is crucial. The technique offers several advantages over conventional approaches:
- Biological Reconstruction: Provides both structural support and blood supply to the necrotic lunate.
- Potential Disease Modification: May halt the progression of avascular necrosis and prevent further collapse.
- Preservation of Natural Anatomy: Maintains normal carpal relationships and biomechanics.
- Avoidance of Salvage Procedures: May prevent the need for more drastic surgeries like proximal row carpectomy or wrist fusion.
Contraindications and Limitations
Despite its benefits, vascularized bone grafting is not suitable for all patients with Kienbock’s disease:
- Advanced Stages (Stage IV): When significant degenerative changes are present throughout the wrist
- Technical Demands: Requires microsurgical expertise and equipment
- Recovery Period: Longer rehabilitation compared to some alternative procedures
- Limited Evidence Base: Long-term outcomes still being established through research
Comparison with Alternative Treatments
For Stage 3A Kienbock’s disease, the main treatment alternatives include:
- Proximal Row Carpectomy (PRC):
- Advantages: Reliable pain relief, maintained motion
- Disadvantages: Loss of carpal height, potential grip weakness, non-reversible
- Limited Wrist Fusion:
- Advantages: Stable construct, pain relief
- Disadvantages: Reduced wrist motion, potential non-union
- Vascularized Bone Graft:
- Advantages: Preserves native anatomy, biological solution, reversible
- Disadvantages: Technical complexity, variable outcomes
The selection of vascularized bone grafting in this case reflects a treatment philosophy prioritizing anatomical preservation and function, particularly appropriate for a young patient.
Clinical Implications
This case demonstrates several important points for practitioners:
- Early Diagnosis: Recognition of Kienbock’s disease before advanced collapse is crucial for preserving treatment options.
- Stage-Appropriate Treatment: Surgical approach should be tailored to the disease stage, patient age, and functional demands.
- Microsurgical Advances: Techniques previously considered experimental are increasingly becoming viable options with experienced surgical teams.
- Team Approach: Collaboration between hand surgeons, radiologists, and rehabilitation specialists optimizes outcomes.
Conclusion
Vascularized bone grafting represents an advanced approach for managing Kienbock’s disease that aims to restore both structure and blood supply to the affected lunate. This case illustrates the successful application of a 4+5 extensor compartmental artery-based vascularized bone graft in a young patient with Stage 3A disease, resulting in pain relief and return to function without resorting to more radical salvage procedures.
The complexity of the procedure necessitates specialized training and expertise, but in appropriate cases and experienced hands, it offers the potential to halt disease progression while preserving wrist anatomy and function. As microsurgical techniques continue to evolve, such reconstructive approaches may become increasingly important in the treatment algorithm for Kienbock’s disease and other conditions characterized by avascular necrosis.
This case adds to the growing body of evidence supporting the role of vascularized bone grafting in the management of selected cases of advanced Kienbock’s disease, offering hope for improved outcomes in this challenging condition.