Introduction
Ischemic colitis represents a significant challenge in gastrointestinal surgery, particularly when complicated by multiple perforations. This condition occurs when blood flow to the colon is reduced to a level insufficient to maintain normal cellular function, leading to inflammation and potentially tissue death. While ischemic colitis is more commonly seen in elderly patients with atherosclerotic disease, its occurrence in younger individuals is rare and often associated with unusual underlying conditions.
This case study presents the successful emergency management of a 32-year-old male patient with severe ischemic colitis complicated by multiple colonic perforations at Burjeel Hospital in Sharjah. The case highlights the importance of prompt recognition, appropriate diagnostic workup, and decisive surgical intervention in managing this potentially fatal condition.
Understanding Ischemic Colitis
Pathophysiology
Ischemic colitis results from inadequate blood flow to the colon, which can occur through several mechanisms:
- Occlusive disease: Blockage of arteries or veins by thrombi, emboli, or external compression
- Non-occlusive ischemia: Low flow states due to systemic hypoperfusion, vasospasm, or shunting
- Venous thrombosis: Impaired venous drainage leading to congestion and secondary arterial insufficiency
The colon is particularly vulnerable to ischemia due to its relatively precarious blood supply, especially at the “watershed” areas where different vascular territories meet, such as the splenic flexure and rectosigmoid junction.
Clinical Presentation
The presentation of ischemic colitis varies widely depending on the severity and extent of ischemia:
- Mild cases: May present with crampy abdominal pain, urgency, and bloody diarrhea
- Moderate cases: More severe pain, peritoneal signs limited to the affected area, and systemic inflammatory response
- Severe cases: Peritonitis, septic shock, and multi-organ failure due to transmural necrosis and perforation
Etiology
While atherosclerosis is the most common underlying cause in elderly patients, other potential etiologies include:
- Cardiac arrhythmias and low output states
- Vasculitis and hypercoagulable states
- Medications (vasoconstrictors, estrogens, danazol)
- Vascular interventions and surgery
- Coagulopathies (inherited or acquired)
- Mechanical obstruction of mesenteric vessels
Case Presentation
Patient Profile and Initial Presentation
A 32-year-old male patient presented to the Emergency Department at Burjeel Hospital, Sharjah, with complaints of recurrent attacks of abdominal pain accompanied by vomiting. The pain was generalized but with particular tenderness in the left side of the abdomen. This was an unusual presentation for a young adult male without significant past medical history.
Initial Diagnostic Workup
The patient was admitted for further evaluation. Magnetic Resonance Imaging (MRI) of the abdomen revealed diffuse multifocal areas of wall edema with mild wall thickening and surrounding fat stranding involving the descending colon. These areas showed mild enhancement on post-contrast images. The radiological features suggested colitis, and a colonoscopy was recommended for further evaluation.
Initial Management and Clinical Course
The patient was started on medical management, including intravenous fluids, bowel rest, and appropriate antibiotics. He showed clinical improvement and was discharged after three days of inpatient treatment.
However, the improvement was short-lived. Just five days after discharge, the patient returned to the Emergency Department with severe abdominal pain and generalized tenderness, suggesting a significant deterioration in his condition.
Advanced Imaging and Preoperative Diagnosis
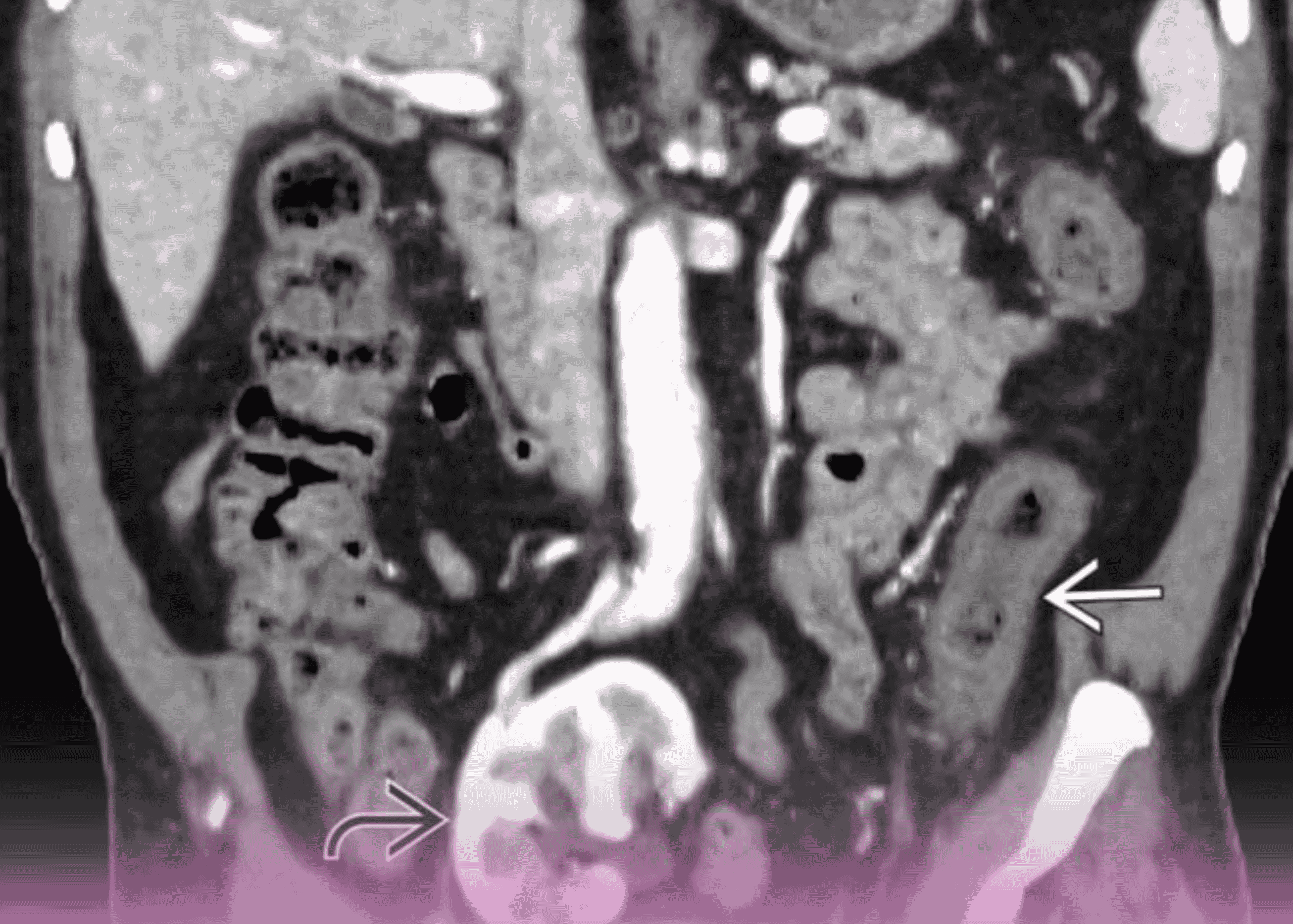
A contrast-enhanced CT scan of the abdomen and pelvis was performed urgently. The scan revealed a clustered loop of small bowel (jejunal loops) with bowel loops located lateral and anterior to the ascending colon, associated with a pulled branch of mesenteric vessels. There was evidence of a possible defect in the mesentery. These findings suggested the possibility of a transmesenteric (internal) hernia.
Based on the patient’s clinical deterioration and the concerning CT findings, the decision was made to proceed with emergency surgery.
Surgical Management
Operative Findings
The patient underwent emergency laparotomy, which revealed critical findings not fully appreciated on preoperative imaging:
- Free fluid in the peritoneal cavity, indicative of peritonitis
- Multiple areas of necrosis and perforation affecting several segments of the colon:
- Hepatic flexure
- Transverse colon
- Part of the descending colon
These findings represented a severe case of ischemic colitis with multiple perforations, a life-threatening condition requiring immediate intervention.
Surgical Procedure
Given the extent and severity of the colonic involvement, the surgical team led by Dr. Mohamed Eraki, Consultant General and Laparoscopic Surgeon and Head of the Surgery Department at Burjeel Hospital, Sharjah, performed the following procedure:
- Extended Colectomy: Resection of the affected bowel segments, including the ascending colon, transverse colon, and part of the descending colon
- Temporary Stoma Creation: A right-sided colostomy was created to divert the fecal stream
- Mucous Fistula: A left-sided mucous fistula was fashioned from the distal bowel segment
- Thorough Lavage: The abdominal cavity was thoroughly irrigated to reduce bacterial contamination
- Drainage: Two large drains were placed to monitor for potential postoperative complications
Postoperative Care
Following surgery, the patient was transferred to the Intensive Care Unit for close monitoring and management of potential septic complications. The postoperative course was successful, with gradual recovery of bowel function and overall clinical improvement. The patient was eventually discharged from the hospital in stable condition.
Diagnostic Investigation and Case Conclusion
Following recovery, a comprehensive workup was initiated to identify the underlying cause of this unusual case of ischemic colitis in a young adult. After detailed investigations, it was discovered that the patient had a congenital coagulopathy (a hereditary blood clotting disorder), which was determined to be the most likely etiology for his ischemic colitis.
This finding highlighted the importance of considering uncommon causes of ischemia in younger patients without traditional risk factors for vascular disease. Congenital coagulopathies can create a hypercoagulable state, predisposing to thrombosis in the mesenteric vessels and subsequent ischemic damage to the bowel.
Discussion
Clinical Significance
This case illustrates several important clinical points:
- Atypical Presentation: Ischemic colitis in young adults is rare and should prompt investigation for unusual underlying causes such as hypercoagulable states, vasculitis, or vascular anomalies.
- Diagnostic Challenges: The initial presentation and imaging findings were suggestive of colitis but did not immediately reveal the severity of the condition. The patient’s rapid deterioration after initial improvement highlights the potentially progressive nature of ischemic bowel disease.
- Surgical Decision-Making: The case demonstrates the critical importance of timely surgical intervention in cases of suspected bowel ischemia. Delaying surgery when peritoneal signs are present can significantly increase morbidity and mortality.
- Role of Extended Colectomy: In cases of extensive colonic ischemia with multiple perforations, extended colectomy with temporary diversion is often necessary to control sepsis and remove all compromised tissue.
Congenital Coagulopathy and Ischemic Colitis
The association between congenital coagulopathies and ischemic colitis merits special attention. Various hereditary thrombophilias can predispose to arterial and venous thrombosis in the mesenteric circulation:
- Factor V Leiden mutation
- Prothrombin gene mutation
- Protein C or S deficiency
- Antithrombin III deficiency
- Hyperhomocysteinemia
In patients with these conditions, even minor reductions in mesenteric blood flow that might be well-tolerated in individuals with normal coagulation can trigger a cascade of thrombosis, ischemia, and tissue necrosis. This underscores the importance of considering hereditary thrombophilias in the differential diagnosis of ischemic colitis, particularly in younger patients without other risk factors.
Surgical Approach to Ischemic Colitis with Perforation
The surgical management of ischemic colitis with perforation follows several key principles:
- Control of Contamination: Removing the perforated bowel and lavaging the peritoneal cavity to reduce bacterial load and minimize septic complications.
- Complete Resection of Non-Viable Tissue: Ensuring all ischemic segments are removed, often requiring assessment of tissue viability through direct inspection, assessment of bleeding at cut edges, and sometimes intraoperative Doppler assessment.
- Damage Control Strategy: In critically ill patients, a staged approach may be necessary, with initial resection and diversion followed by later restoration of intestinal continuity once the patient is stabilized.
- Temporary Fecal Diversion: Creating a stoma to protect any anastomosis or to simplify the initial procedure when the patient is unstable. This is often essential in cases of fecal peritonitis to prevent further contamination.
In this case, the extended colectomy with end stoma and mucous fistula creation represents the application of these principles, prioritizing the patient’s survival in a life-threatening situation.
Postoperative Considerations
Short-term Management
Following surgery for ischemic colitis with multiple perforations, several aspects of care are critical:
- Hemodynamic Stabilization: Maintaining adequate perfusion to prevent further ischemic damage to other organs
- Broad-Spectrum Antibiotics: Continued administration to control polymicrobial intra-abdominal infection
- Nutritional Support: Early initiation of nutrition to support wound healing and immune function
- Thromboprophylaxis: Given the underlying hypercoagulable state, appropriate anticoagulation is essential once bleeding risk is controlled
- Stoma Management: Early involvement of stoma care specialists to optimize adaptation and prevent complications
Long-term Planning
Once recovered from the acute event, several considerations come into play:
- Investigation and Management of Underlying Coagulopathy: Detailed hematological evaluation and long-term management plan, potentially including anticoagulation therapy
- Restoration of Intestinal Continuity: Assessment for potential stoma reversal and colocolonic or ileocolonic anastomosis, typically considered after 3-6 months
- Surveillance: Regular follow-up to monitor for recurrent ischemia or other complications
- Quality of Life Considerations: Addressing the psychological and social impact of temporary or permanent stoma
Future Perspectives
Advancements in Diagnostics
Earlier diagnosis of ischemic colitis could potentially prevent the severe complications seen in this case. Several emerging modalities may help in this regard:
- Biomarkers: Intestinal fatty acid binding protein (I-FABP), citrulline, and D-lactate have shown promise as early markers of intestinal ischemia
- Advanced Imaging: CT angiography protocols specifically optimized for mesenteric vasculature can improve detection of early ischemic changes
- Colonoscopic Assessment: Early endoscopic evaluation with modalities like narrow-band imaging might improve visualization of mucosal ischemic changes
Therapeutic Innovations
Evolving therapeutic approaches that may improve outcomes in ischemic colitis include:
- Endovascular Interventions: Balloon angioplasty or stenting of mesenteric vessels in cases of occlusive disease
- Novel Anticoagulants: Direct oral anticoagulants may offer advantages over traditional therapy for patients with thrombophilia
- Targeted Therapies: Agents specifically addressing the inflammatory cascade in ischemia-reperfusion injury
Conclusion
This case of ischemic colitis with multiple perforations in a young patient with underlying congenital coagulopathy illustrates the importance of considering uncommon etiologies in atypical presentations. The successful outcome highlights the value of prompt surgical intervention with appropriate resection and temporary diversion in managing this life-threatening condition.
For clinicians, this case reinforces several key lessons:
- Ischemic colitis should be included in the differential diagnosis of acute abdominal pain even in younger patients without typical risk factors
- Rapid deterioration can occur in ischemic colitis, necessitating close monitoring and low threshold for surgical intervention
- Extended colectomy with temporary diversion represents an appropriate damage-control approach in cases with multiple perforations
- Underlying coagulopathies should be investigated in cases of ischemic colitis without obvious etiology, particularly in younger patients
The successful management of this complex case at Burjeel Hospital Sharjah demonstrates the high level of surgical expertise and comprehensive care available at the institution, enabling effective treatment of rare and life-threatening conditions.