Understanding a Life-Threatening Gastrointestinal Emergency
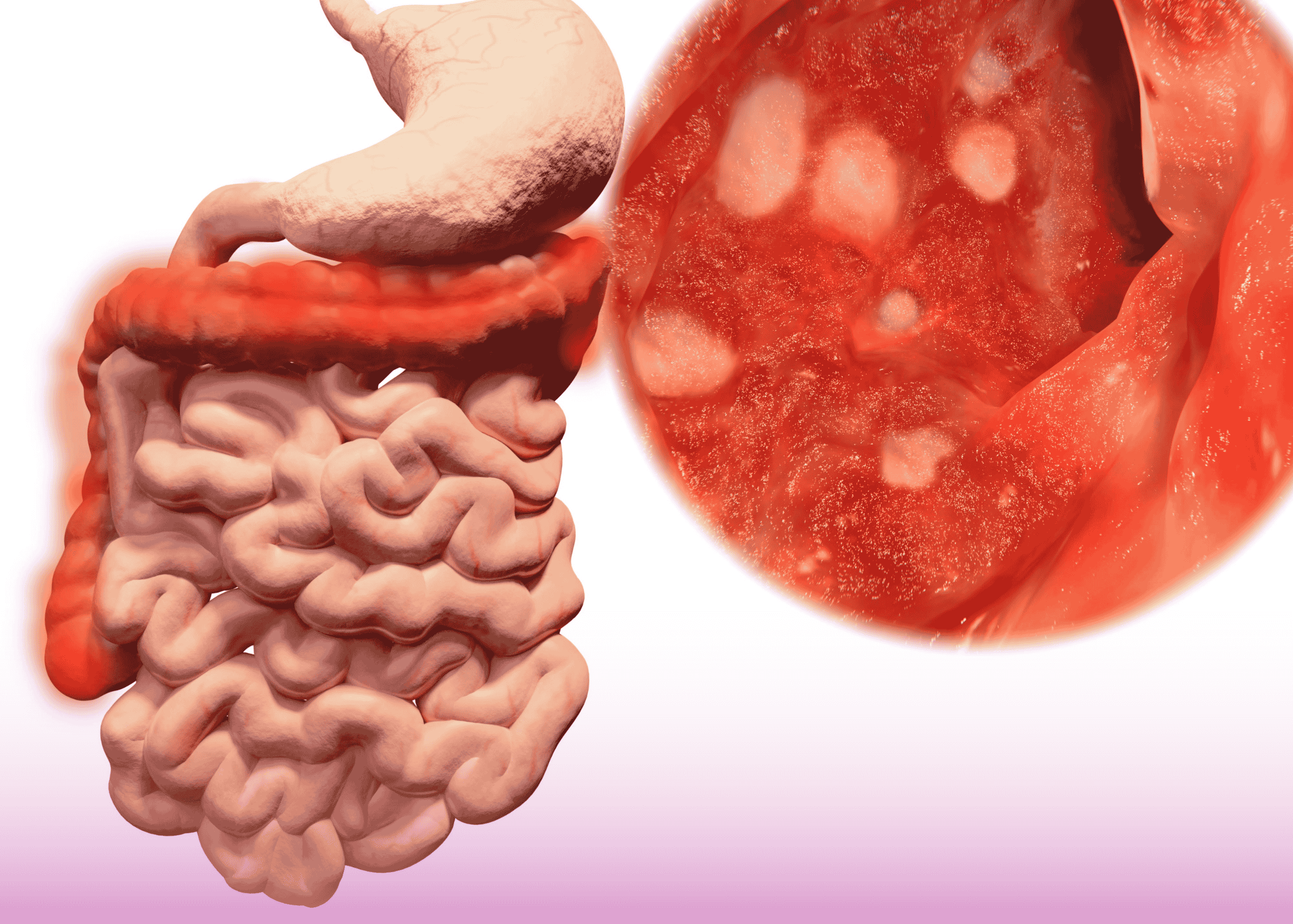
Ischemic colitis represents the most common form of gastrointestinal ischemia, occurring when blood flow to the colon becomes compromised, leading to tissue damage ranging from superficial mucosal injury to full-thickness transmural necrosis. While many cases of ischemic colitis can be managed conservatively, the development of multiple colonic perforations represents a life-threatening surgical emergency requiring prompt intervention. A recent case at Burjeel Hospital highlights the critical importance of early recognition and aggressive surgical management in this challenging clinical scenario.
The Clinical Presentation: From Subtle Symptoms to Systemic Sepsis
The patient in this case presented with what initially appeared to be a routine case of ischemic colitis, with symptoms including:
- Progressive abdominal pain, initially cramping but becoming more severe and diffuse
- Bloody diarrhea
- Nausea and vomiting
- Low-grade fever
- Progressive abdominal distension
What distinguished this case from more typical presentations of ischemic colitis was the rapid clinical deterioration, with the development of signs of peritonitis, including:
- Rebound tenderness and guarding
- Absent bowel sounds
- Progressive hemodynamic instability
- Rising inflammatory markers (leukocytosis, elevated C-reactive protein)
- Metabolic acidosis
These findings raised immediate concern for colonic perforation as a complication of severe transmural ischemia, representing a surgical emergency requiring prompt intervention.
Diagnostic Approach: Rapid Assessment for Optimal Management
The diagnostic workup for suspected ischemic colitis with perforation must be expedited to enable timely surgical intervention. In this case, the diagnostic approach included:
Laboratory Studies
- Complete blood count revealing leukocytosis with left shift
- Comprehensive metabolic panel showing electrolyte abnormalities
- Elevated lactate level suggesting tissue ischemia
- Coagulation studies to assess for hypercoagulable states
Imaging Studies
- Abdominal X-ray demonstrating free air under the diaphragm, indicative of perforation
- CT scan of the abdomen and pelvis with intravenous contrast revealing:
- Segmental thickening of the colonic wall, particularly involving the splenic flexure and descending colon
- Pneumoperitoneum consistent with perforation
- Multiple sites of discontinuity in the colonic wall indicating multiple perforations
- Surrounding inflammatory changes and free fluid
The combination of clinical findings and imaging studies confirmed the diagnosis of ischemic colitis complicated by multiple perforations, necessitating immediate surgical intervention.
Surgical Management: Principles and Approach
The management of perforated ischemic colitis requires a systematic approach focused on:
- Aggressive Resuscitation:
- Fluid resuscitation with crystalloids and colloids
- Vasopressor support as needed
- Correction of electrolyte abnormalities
- Initiation of broad-spectrum antibiotics to cover gram-negative and anaerobic organisms
- Prompt Surgical Intervention:
- Exploratory laparotomy to assess the extent of disease
- Resection of all nonviable bowel segments
- Assessment of vascular supply to remaining intestine
- Decision-making regarding primary anastomosis versus ostomy creation
- Postoperative Care:
- Continued intensive care monitoring
- Nutritional support
- Wound management
- Prevention of complications including thromboembolism
The Operative Findings and Surgical Decision-Making
Upon exploratory laparotomy, the surgical team encountered:
- Extensive purulent peritonitis throughout the abdominal cavity
- Multiple perforations primarily involving the splenic flexure and descending colon
- Transmural necrosis extending from the mid-transverse colon to the sigmoid colon
- Relatively sparing of the right colon and rectum
- No evidence of occlusive vascular disease in the major mesenteric vessels
Based on these findings, the surgical team headed by Burjeel Hospital, Sharjah’s, Medical Director and Consultant General, Laparoscopic Surgery and Oncosurgery, Dr. Mohamed El Sayed Eraki Ibrahium proceeded with:
- Extended Left Hemicolectomy: Resection of the affected colonic segments, including the distal transverse colon, splenic flexure, descending colon, and proximal sigmoid colon
- End Colostomy Creation: Given the presence of peritonitis and the compromised tissue quality, the decision was made to avoid primary anastomosis and instead create an end colostomy (Hartmann’s procedure) with a distal rectal stump
- Thorough Peritoneal Lavage: Copious irrigation with warm saline to clear purulent material and reduce bacterial burden
- Drain Placement: Strategic placement of drains to monitor for ongoing leakage or abscess formation
Pathological Findings: Confirming the Diagnosis
The resected colonic specimen was sent for pathological examination, which revealed:
- Transmural ischemic necrosis with multiple areas of perforation
- Vascular congestion and hemorrhage within the bowel wall
- Inflammatory infiltrate consistent with acute ischemic injury
- Microvascular thrombosis in small vessels of the colonic wall
- No evidence of vasculitis, malignancy, or infectious etiology
These findings confirmed the diagnosis of severe ischemic colitis with multiple perforations, likely related to non-occlusive mesenteric ischemia.
Postoperative Course and Outcome
The immediate postoperative period was characterized by:
- Continued intensive care support with mechanical ventilation and hemodynamic monitoring
- Gradual resolution of sepsis with appropriate antibiotic therapy
- Progressive improvement in inflammatory markers
- Initiation of enteral nutrition on postoperative day 4
- Stoma function beginning on postoperative day 3
The patient was discharged from the intensive care unit on postoperative day 7 and from the hospital on postoperative day 14. Following a period of recovery and nutritional optimization, the patient would be evaluated for potential colostomy reversal, typically considered 3-6 months after the initial procedure.
Risk Factors and Preventive Strategies
Several factors may increase the risk of ischemic colitis and subsequent perforation:
- Advanced age and atherosclerotic vascular disease
- Cardiac arrhythmias, particularly atrial fibrillation
- Recent major cardiovascular surgery
- Severe heart failure or hypotension
- Hypercoagulable states
- Vasopressor use
- Certain medications including NSAIDs and hormone replacement therapy
- Chronic obstructive pulmonary disease
Preventive strategies for high-risk patients include:
- Optimization of cardiac output and blood pressure
- Careful management of fluid status
- Anticoagulation when appropriate
- Cautious use of vasopressors
- Monitoring for abdominal symptoms in patients with risk factors
Learning Points and Clinical Significance
This challenging case highlights several important clinical lessons:
- Early Recognition Is Critical: The progression from mucosal ischemia to transmural necrosis and perforation can be rapid, emphasizing the importance of vigilant monitoring and early recognition of deterioration.
- Imaging is Essential: CT imaging plays a crucial role in diagnosing ischemic colitis complicated by perforation and guiding surgical decision-making.
- Resuscitation Before and During Surgery: Aggressive fluid resuscitation, antibiotics, and hemodynamic support are essential components of management.
- Surgical Principles: In the setting of multiple perforations and peritonitis, resection of all affected segments with diversion (stoma creation) is generally preferred over primary anastomosis.
- Multidisciplinary Approach: Optimal management requires collaboration between emergency physicians, surgeons, intensivists, and interventional radiologists.
Conclusion: The Importance of Timely Intervention
Ischemic colitis with multiple perforations represents a life-threatening surgical emergency requiring prompt diagnosis and intervention. This case from Burjeel Hospital demonstrates that with early recognition, appropriate imaging, and timely surgical management, even patients with this severe complication can achieve favorable outcomes.
The multidisciplinary approach employed in this case, along with adherence to fundamental surgical principles for managing perforated viscus, illustrates the high level of care available for complex gastrointestinal emergencies at Burjeel’s surgical facilities.