Introduction
Intussusception, a condition where one segment of the intestine telescopes into an adjacent segment, is predominantly seen in children but rarely occurs in adults. When it does appear in adults, it presents unique diagnostic and treatment challenges that require careful consideration. This case study examines an unusual presentation of ileocolic intussusception in a middle-aged patient and highlights the importance of prompt surgical intervention.
Patient Presentation
A previously healthy 56-year-old woman presented to the emergency department with a two-day history of concerning gastrointestinal symptoms. Her chief complaints included:
- Lower abdominal pain that had progressively worsened
- Multiple episodes of vomiting
- Constipation with no bowel movements for two days
These symptoms had developed suddenly with no apparent trigger, leading to her seeking medical attention after conservative measures at home failed to provide relief.
Diagnostic Journey
Initial Assessment
Upon presentation, the patient appeared uncomfortable but had stable vital signs. Physical examination revealed tenderness in the lower right quadrant of the abdomen with mild distension. The initial clinical impression suggested a possible bowel obstruction, necessitating further investigation.
Laboratory Findings
Blood work demonstrated a mild elevation of inflammatory markers:
- Slightly elevated white blood cell count
- Moderately increased C-reactive protein levels
- Other laboratory parameters remained within normal ranges
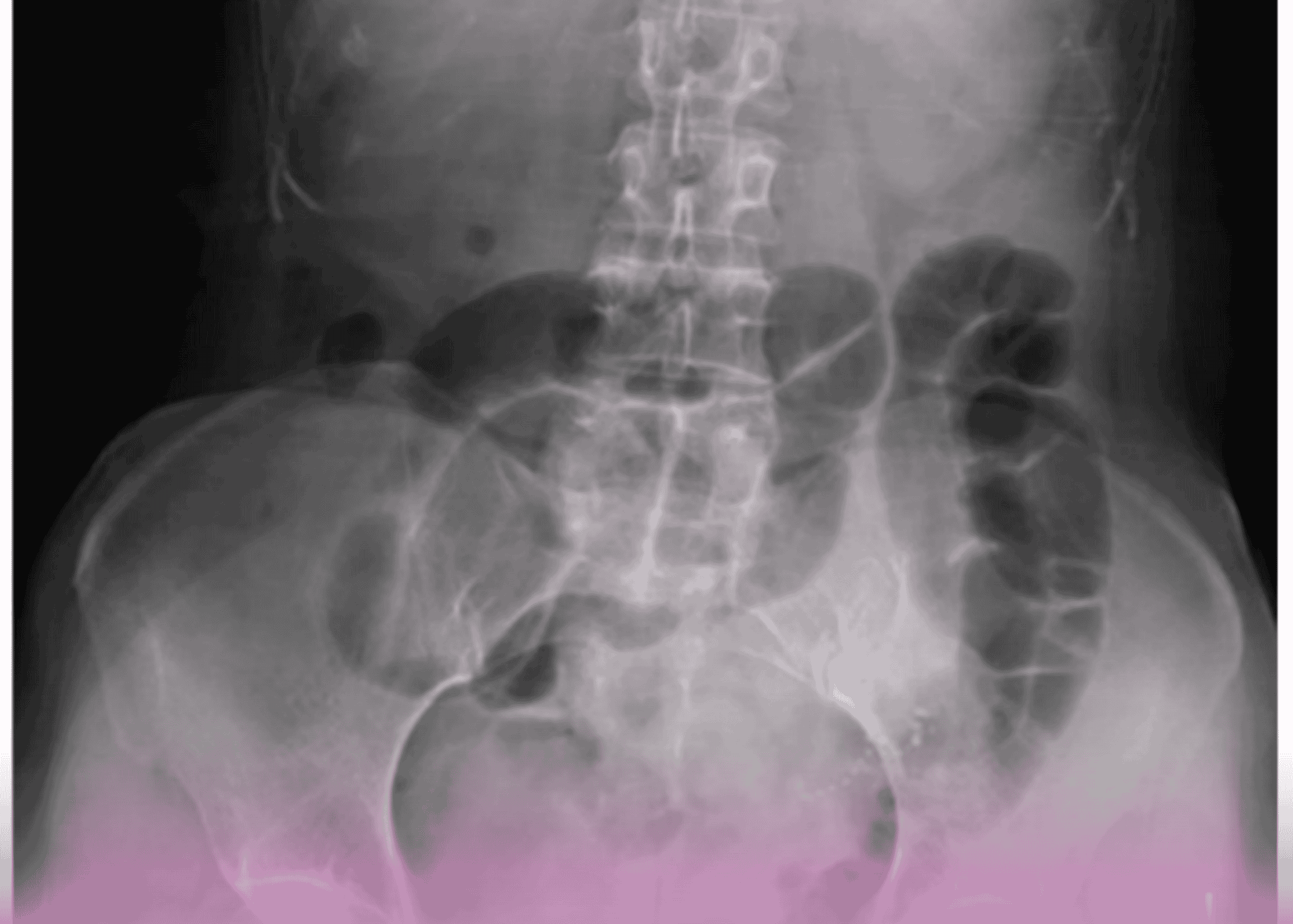
Imaging Studies
A computed tomography (CT) scan of the abdomen and pelvis proved crucial for diagnosis, revealing:
- Classic “target sign” indicating ileocecal intussusception
- Proximally dilated small bowel loops suggestive of partial obstruction
- No evidence of perforation or ischemia
Based on these findings, a diagnosis of ileocolic intussusception was established, and the patient was prepared for urgent surgical intervention.
Surgical Management
Given the patient’s age and the rarity of intussusception in adults, the surgical team approached the case with careful consideration that the condition likely had a pathological lead point.
Operative Approach
The patient underwent laparotomy, which confirmed the preoperative diagnosis of ileocolic intussusception. The surgical procedure involved:
- Careful manual reduction of the intussusception
- Identification of a large, smooth-surfaced, rubbery ileal polyp as the lead point
- Ileocecal resection with primary ileocolic anastomosis
The decision for bowel resection rather than simple reduction was based on the understanding that adult intussusception typically has a pathological lead point that requires removal.
Histopathological Findings
Examination of the resected specimen confirmed:
- A benign ileal polyp measuring approximately 3.5 cm in diameter
- No evidence of dysplasia or malignancy
- Normal surrounding mucosa
These findings validated the surgical approach and provided reassurance regarding the patient’s prognosis.
Post-Operative Course
The patient’s recovery proceeded smoothly with:
- Gradual return of bowel function on the second postoperative day
- Successful transition from intravenous to oral nutrition
- Adequate pain control with standard analgesics
- No postoperative complications
She was discharged home on the fourth postoperative day with appropriate follow-up arrangements and dietary guidance.
Discussion
Uniqueness of Adult Intussusception
This case highlights several important aspects of adult intussusception:
- Epidemiological rarity: While common in children, intussusception accounts for only 1-5% of all cases of intestinal obstruction in adults.
- Etiology differences: Unlike pediatric cases that are usually idiopathic, adult intussusception nearly always has a pathological lead point, which in this case was a benign ileal polyp.
- Surgical management: The standard approach in adults is resection rather than reduction alone due to the high likelihood of pathological lead points and potential for malignancy.
Diagnostic Challenges
Diagnosing adult intussusception can be challenging due to:
- Non-specific symptoms that can mimic other abdominal conditions
- Chronic, intermittent presentations in some cases
- Varying clinical presentations depending on location and duration
In this case, the acute presentation and comprehensive imaging studies facilitated timely diagnosis and intervention.
Surgical Considerations
The surgical management of this case illustrates important decision-making factors:
- Assessment of the lead point’s nature during surgery
- Determining appropriate extent of resection
- Balancing oncological principles with preservation of bowel length
The confirmation of a benign pathology justified the limited resection performed.
Conclusion
This case demonstrates the successful management of adult ileocolic intussusception caused by a benign ileal polyp. Despite being uncommon in adults, intussusception should remain in the differential diagnosis for patients presenting with bowel obstruction symptoms. The case underscores the importance of prompt surgical intervention and careful pathological assessment in adult intussusception cases.
The patient’s smooth recovery and uncomplicated postoperative course highlight the effectiveness of timely surgical management. This case, managed by Dr. Talat Shaban Abdullah Al-Shaban, Consultant General Surgeon specializing in minimally invasive laparoscopic and robotic surgery , represents a textbook example of the proper approach to adult intussusception.
Key Learning Points
- Adult intussusception is rare but should be considered in the differential diagnosis for bowel obstruction.
- CT scanning is the imaging modality of choice for diagnosis.
- Unlike in children, adult intussusception typically requires surgical resection rather than simple reduction.
- Identifying the nature of the lead point is crucial for determining the extent of surgical resection.
- Most adult intussusceptions have an identifiable lead point, which can range from benign polyps to malignant lesions.