Mr. S, a 63-year-old male, presented with a history of progressive abdominal distension spanning 8 years, intensifying notably over the past 6 months. His symptoms included severe discomfort, disrupted sleep patterns, and recent bilateral pedal edema extending up to the knee joints. Additionally, he reported experiencing severe back pain that significantly impeded his daily activities.
Clinical examination revealed bilateral pedal edema and a massively distended and tense abdomen. A large mass measuring 50x50x40 cm occupied all quadrants of the abdomen, causing vertical stretching of the umbilicus. Lower abdominal wall edema was also observed. Despite the massive tumor burden, bilateral scrotal gonads were normal, and no palpable left supraclavicular nodes were detected.
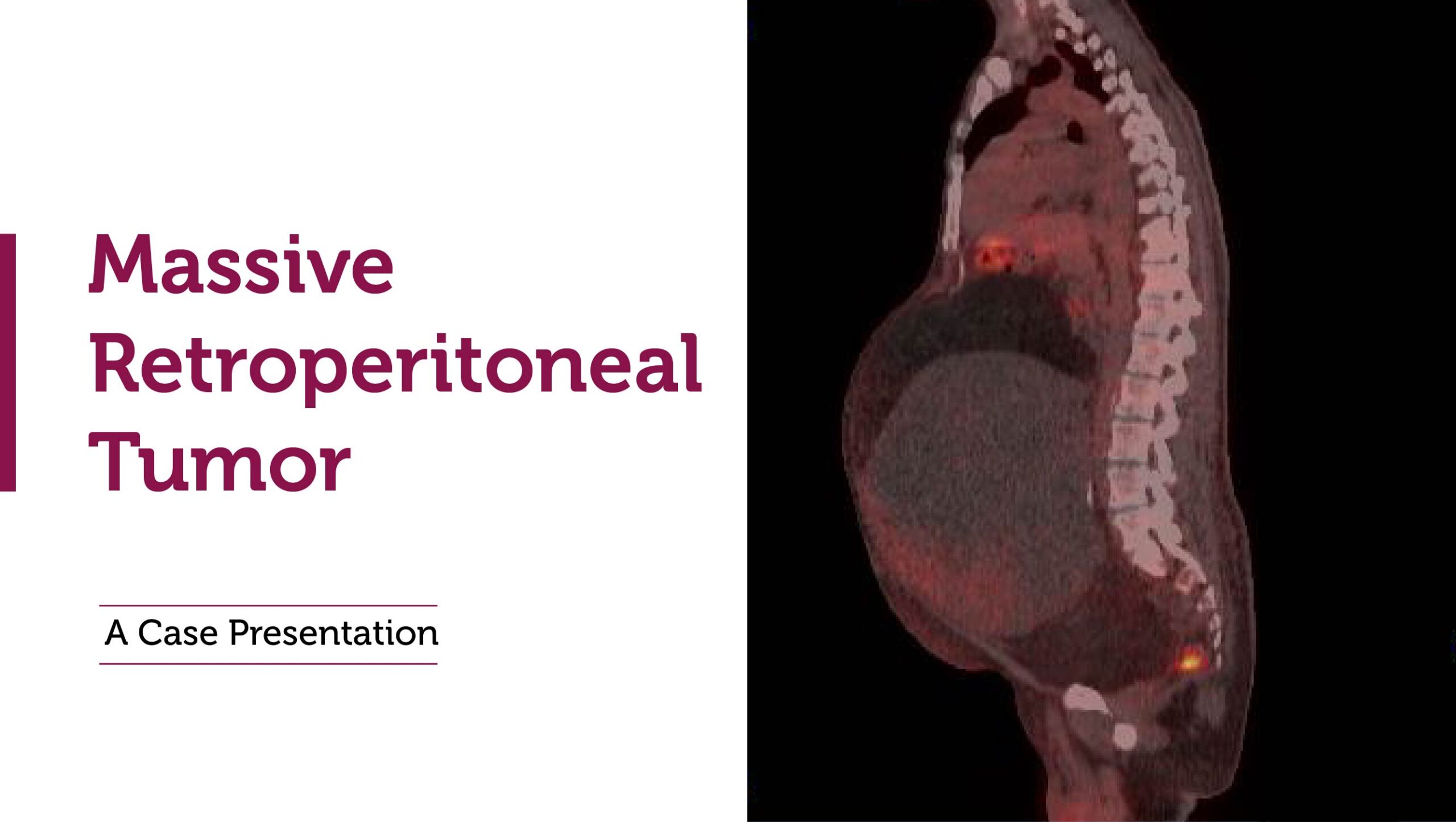
Diagnostic imaging, including a Contrast-Enhanced Computed Tomography (CECT) of the abdomen, depicted a large heterogeneous mass with fatty, solid, and calcified components. The tumor displaced bowel loops superiorly and compressed the aorta and inferior vena cava (IVC). The urinary bladder was displaced laterally due to the mass’s size and location within the retroperitoneal space. Subsequent PET CT confirmed the absence of distant metastases.
Laboratory investigations, including tumor markers such as AFP, Beta HCG, LDH, CEA, and CA 19-9, were within normal limits, indicating no evidence of metastatic spread.
A multidisciplinary tumor board, comprising oncologists, surgeons, radiologists, and nuclear medicine specialists, recommended surgical intervention due to the tumor’s size and associated symptoms. On June 4th, 2024, Mr. S underwent a complex laparotomy for excision of the retroperitoneal tumor following bilateral ureteric catheterization. The intricate procedure lasted 5 hours and involved a surgical team led by Dr. Mohammed Basheeruddin Inamdar, Consultant Surgical Oncologist, supported by Dr. Omar Hnaidi, Consultant Urology, and Dr. Mohammed Eid Ali, Consultant Anesthesia. The surgery addressed challenges such as severe compression on major vessels (IVC, Aorta) caused by the massive tumor.
Postoperatively, Mr. S experienced minimal blood loss and a smooth recovery, leading to discharge on the 6th day after surgery. The procedure significantly alleviated his symptoms and improved his quality of life.
This case highlights the critical role of multidisciplinary collaboration in managing rare and complex tumors like retroperitoneal liposarcomas. It underscores the importance of early diagnosis and timely surgical intervention to optimize patient outcomes and restore functional health.