Introduction
A recent case at Burjeel Royal Hospital Asharej highlights the importance of considering tropical parasitic infections in the differential diagnosis of urological symptoms, especially in patients with relevant travel or exposure history. This complex case demonstrates the multidisciplinary approach required for diagnosing and treating schistosomiasis, a condition that can often be overlooked in initial evaluations.
Patient Presentation
A 41-year-old male patient sought medical attention for persistent abdominal and right flank pain, accompanied by gross hematuria and intermittent nausea over several weeks. Notably, the patient reported a previous episode of gross hematuria two years prior that had spontaneously resolved without medical intervention. Despite these concerning urinary symptoms, the patient described himself as generally healthy with no significant medical history.
Initial Investigations
The diagnostic journey began with ultrasound imaging, which revealed dilation of the right renal pelvis. Further evaluation with CT scanning of the abdomen and pelvis identified:
- A 5 x 4 mm calculus in the distal right ureter
- A smaller calculus at the vesico-ureteric junction
- Diffuse bladder wall thickening
- Non-dependent isodense foci in the bladder lumen, suspected to be blood clots
These findings initially suggested a urolithiasis-related etiology for the patient’s symptoms, with possible secondary inflammation of the bladder wall.
Surgical Intervention and Unexpected Findings
Under the care of Dr. Humam Qaraschouli, Consultant Urologist, the patient underwent ureterorenoscopy (URS) for stone removal and further evaluation of the urinary tract. The procedure was supported by Dr. Maitham Badawy and Dr. Syed Abu Sayeed, Specialists in Anesthesia.
Upon cystoscopic examination, several concerning and unexpected findings were noted:
- Diffuse redness and irritation of the bladder mucosa
- Tumorous changes in the area of the bladder dome and base, raising initial concerns for malignancy
- Characteristic “sandy patches,” a pathognomonic finding in schistosomiasis
During post-operative discussion with the patient and his wife, a critical piece of medical history emerged: the patient had experienced schistosomiasis (bilharzia) during childhood, a fact not disclosed during initial consultations.
Multidisciplinary Approach
Following this revelation, a multidisciplinary approach was initiated:
- The ureteric stones were successfully removed and a DJ stent was placed
- Resection of the affected bladder areas was performed for histopathological examination
- Dr. Maher Wassim Malaeb, Specialist in Gastroenterology and Medical Director, was consulted
- Colonoscopy identified suspected areas of infection in the rectum and sigmoid colon
- Biopsies from both the bladder and intestinal lesions confirmed the diagnosis of schistosomiasis, likely caused by Schistosoma haematobium
Treatment and Follow-up
After removal of the DJ stent, the patient was referred to the Infectious Diseases department for definitive treatment with Praziquantel, the antiparasitic medication of choice for schistosomiasis.
Clinical Significance
This case underscores several important clinical lessons:
- The value of comprehensive history-taking, including childhood illnesses and geographic exposure
- The importance of considering parasitic infections in the differential diagnosis of urological conditions
- The need for multidisciplinary collaboration in complex cases
- The potential for chronic, latent parasitic infections to manifest years after initial exposure
Understanding Schistosomiasis
Schistosomiasis, also known as bilharzia or snail fever, is a parasitic disease caused by flatworms of the genus Schistosoma. It predominantly affects tropical and subtropical regions, particularly in Africa, Asia, and South America.
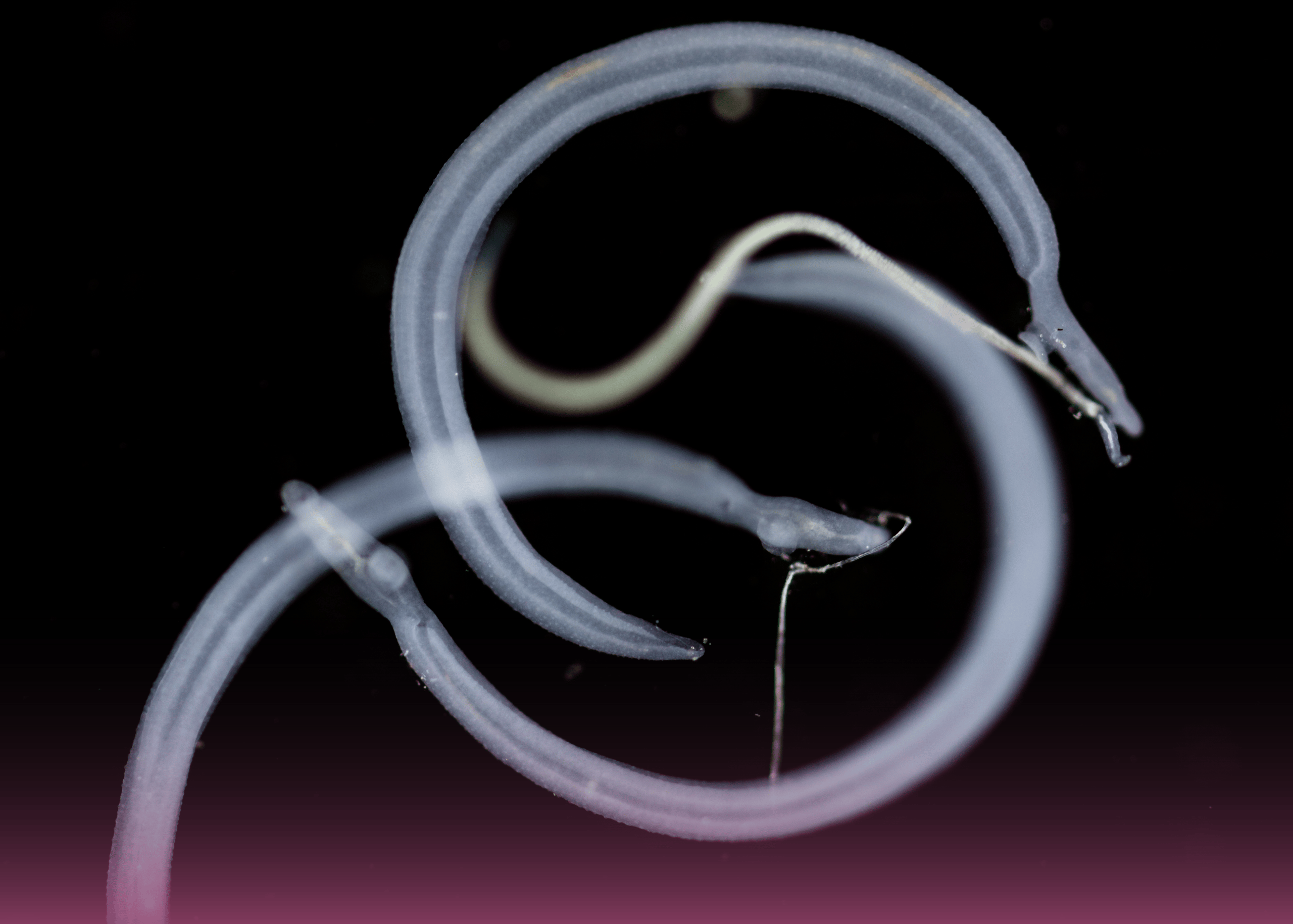
The life cycle involves:
- Parasite eggs released into water bodies through human excretion
- Larval development in freshwater snails
- Release of infective cercariae into water
- Penetration of human skin during water contact
- Migration to target organs where adult worms produce eggs
In urinary schistosomiasis (S. haematobium), eggs trapped in the urinary tract cause inflammation, scarring, and potential long-term complications including bladder cancer.
Conclusion
This case exemplifies the diagnostic challenges and successful management of schistosomiasis at Burjeel Royal Hospital Asharej. By maintaining awareness of tropical diseases even in patients without recent travel history, the medical team was able to identify and appropriately treat this chronic parasitic infection, preventing further complications and providing relief from the patient’s symptoms.