Imagine struggling to breathe for 14 years. Every day marked by chronic cough, breathing difficulties, and fatigue. Missing school, unable to participate in activities other teenagers enjoy, and watching friends run and play while you struggle to catch your breath. This was the reality for a 17-year-old girl whose life was transformed by advanced thoracic surgery.
A Childhood Defined by Illness
The patient first experienced symptoms at age three. What began as severe pneumonia in early childhood progressed into a chronic lung infection that persisted for 14 years. Despite consultations at multiple healthcare facilities, her symptoms continued and worsened, significantly affecting:
- Daily activities
- Academic performance
- Physical abilities
- Quality of life
- Mental well-being
Finally, A Diagnosis
Clinical evaluation revealed the extent of the damage:
- Chronic lung infection with significant damage to the right middle lobe
- Pulmonary function tests showing reduced ventilatory function (FEV1 – 77%, FVC – 88%)
- Imaging showed a destroyed right middle lobe with possible spread of infection to adjacent lung tissue
Final Diagnosis:
- Chronic lung infection with destruction of the right middle lobe (post-pneumonia sequelae)
- Secondary restrictive lung disease due to chronic parenchymal damage
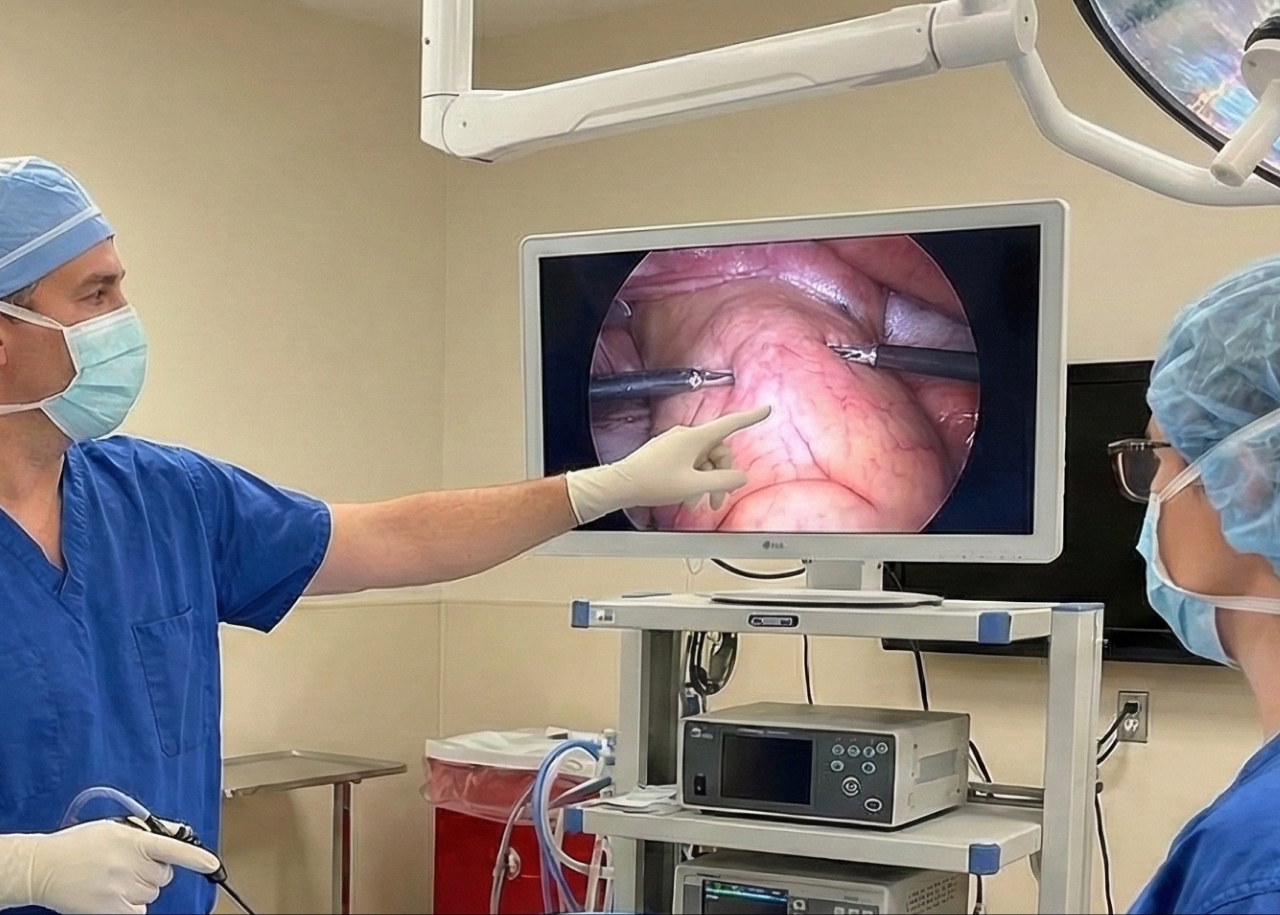
The Surgical Solution: Uni-Portal VATS
After careful patient stabilization, the decision was made: minimally invasive uni-portal Video-Assisted Thoracoscopic Surgery (VATS) for right middle lobectomy.
Why VATS?
- Single small incision instead of large thoracotomy
- Less post-operative pain
- Faster recovery
- Better cosmetic result
- Preserved chest wall function
- Earlier return to normal activities
Anesthetic Challenge: Single-lung ventilation (left lung) during surgery—allowing the surgical team to work on the right lung while maintaining adequate oxygenation.
The Complex Procedure
Operative Approach:
- Minimally invasive uni-portal VATS technique
- Right middle lobectomy (removal of infected, destroyed lung lobe)
- Preservation of healthy lung tissue
- Minimal blood loss
- Precise dissection and removal
Post-Operative Care:
- Chest tube removed on postoperative day 1
- Early mobilization and breathing exercises
- Monitored recovery
Life-Changing Results
The transformation was remarkable:
Immediate Improvements:
- Reduced cough
- Improved breathing capacity
- Increased energy levels
Return to Normal Life:
- Resumed academics
- Started running again
- Began drawing and writing (hobbies previously too exhausting)
- Participated in activities with peers
Follow-up Pulmonary Function Tests: FEV1 – 77%, FVC – 88% (satisfactory recovery despite removal of lung lobe)
Understanding Lung Lobectomy
The lungs are divided into lobes:
- Right lung: 3 lobes (upper, middle, lower)
- Left lung: 2 lobes (upper, lower)
When one lobe is severely damaged by infection or disease, removing it allows:
- Remaining healthy lung tissue to expand
- Elimination of chronic infection source
- Improved overall lung function
- Better quality of life
The body compensates remarkably well:
- Remaining lobes expand
- Breathing capacity improves
- Normal activities resume
- Quality of life significantly enhanced
The Challenges of This Case
1. Long-Standing Misdiagnosis (14 years)
- Patient endured symptoms without definitive diagnosis
- Prolonged morbidity affecting development
- Multiple failed treatment attempts
2. Psychological Impact
- Chronic illness affected mental well-being
- Social isolation from peers
- Anxiety about the future
- Required emotional support before surgery
3. Surgical Complexity
- VATS lobectomy in chronically infected, scarred lung
- Required precise technique
- Risk of complications in damaged tissue
- Need for specialized thoracic surgery expertise
4. Physiological Adaptation
- Post-lobectomy, patient lost approximately 10% lung function
- Remaining lung capacity needed to compensate
- Successful adaptation allowed full recovery
5. Multidisciplinary Approach
- Collaboration between pulmonology, thoracic surgery, and anesthesia
- Coordinated pre-operative optimization
- Specialized post-operative care
- Essential for successful outcome
Why Minimally Invasive Thoracic Surgery Matters
Traditional Open Thoracotomy:
- Large incision between ribs
- Significant post-operative pain
- Longer hospital stay (7-10 days)
- Extended recovery (weeks to months)
- Larger scar
- Reduced chest wall function
Uni-Portal VATS Approach:
- Single small incision
- Minimal pain
- Shorter hospital stay (3-5 days)
- Faster recovery (days to weeks)
- Better cosmetic result
- Preserved chest wall mechanics
- Earlier return to normal activities
The Surgical Precision Required
Uni-portal VATS is technically demanding:
- All instruments through one small incision
- Requires advanced thoracoscopic skills
- Limited centers worldwide offer this expertise
- Especially challenging in chronically infected, scarred tissue
- Demands precise visualization and instrument control
Burjeel’s Advanced Thoracic Surgery Capabilities
- Specialized thoracic surgeons
- Minimally invasive VATS expertise
- Advanced thoracoscopic equipment
- Comprehensive pulmonology services
- Multidisciplinary thoracic disease management
- Pediatric and adult thoracic surgery
- Post-operative rehabilitation programs

Our Experts

Dr. Taj Mohammed Fiyaz Chowdhry
Consultant – Thoracic Surgery
Burjeel Royal Hospital, Al Ain
Advanced Thoracic Surgery
Complex lung conditions require specialized expertise. Our thoracic surgery team provides comprehensive evaluation and advanced minimally invasive surgical solutions.