Significances
Pre-Surgical Preparation
Pre-surgical rehabilitation focuses on strengthening surrounding muscles, improving range of motion, and reducing swelling to optimize knee function and prepare for surgery.
Post-Surgical Recovery
Post-surgical rehabilitation aims to promote healing of the reconstructed ligament, restore knee mobility and stability, and rebuild strength in the affected leg.
Post-Surgical Recovery
Post-surgical rehabilitation aims to promote healing of the reconstructed ligament, restore knee mobility and stability, and rebuild strength in the affected leg.
Functional Restoration
Rehabilitation programs are tailored to the individual’s specific needs and goals, focusing on restoring functional abilities for activities of daily living, work, and sports participation.
Neuromuscular Control
Rehabilitation includes exercises and activities to enhance proprioception, balance, and coordination to reduce the risk of re-injury and improve overall joint stability.
Return to Activity
Rehabilitation progresses through various phases, gradually reintroducing activities such as walking, running, jumping, and cutting maneuvers to safely return to pre-injury levels of activity and sport.
Measures to Support
Pre-Surgical Conditioning
Engage in pre-surgical exercises and physical therapy interventions to strengthen quadriceps, hamstrings, and calf muscles, improve knee range of motion, and optimize overall physical condition.
Post-Surgical Mobilization
Initiate early mobilization and gentle exercises, including ankle pumps, quadriceps sets, and passive range of motion exercises, under the guidance of a physical therapist to reduce stiffness and promote circulation.
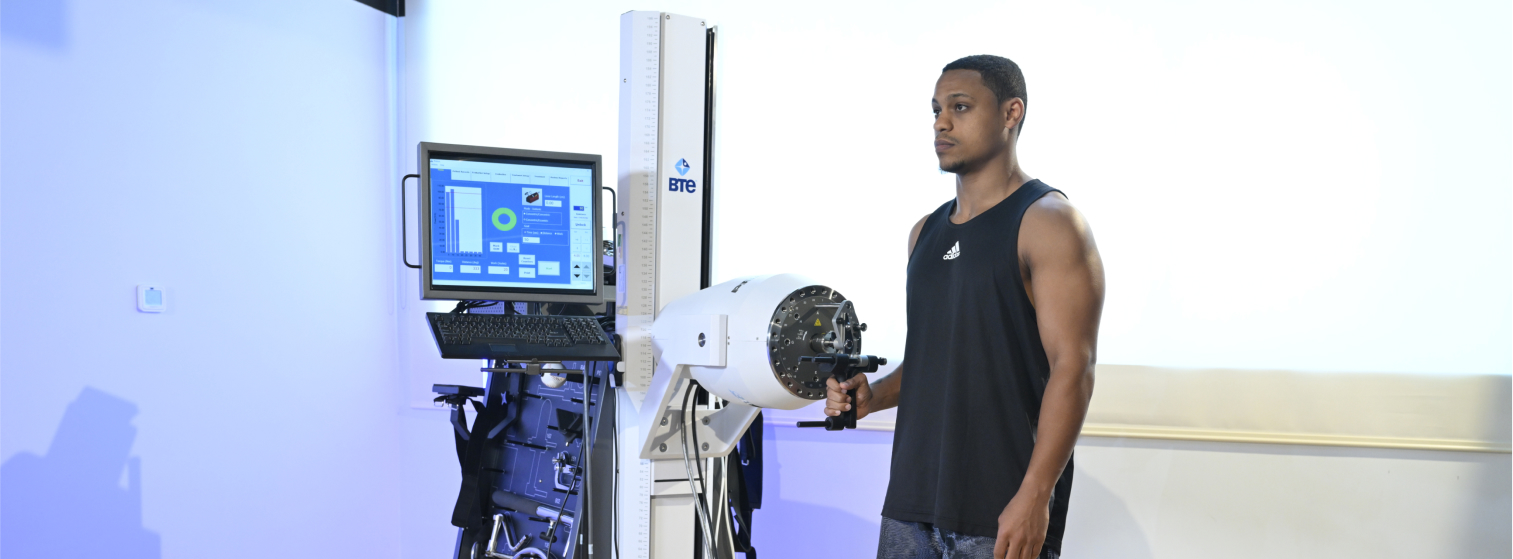
Progressive Exercise Program
Progress through a structured rehabilitation program consisting of exercises to improve strength, flexibility, proprioception, and neuromuscular control, with gradual advancement in intensity and complexity.
Neuromuscular Training
Incorporate neuromuscular training exercises, such as balance drills, agility exercises, and plyometrics, to enhance dynamic stability and reduce the risk of re-injury during sports and activities.
Manual Therapy Techniques
Receive manual therapy interventions, such as joint mobilizations, soft tissue mobilization, and myofascial release, to improve tissue flexibility, reduce scar adhesions, and alleviate pain.
Brace and Support
Utilize a knee brace or supportive device as prescribed by the surgeon or physical therapist to protect the reconstructed ligament, stabilize the knee joint, and provide confidence during early stages of rehabilitation.
Patient Education
Receive education on post-operative precautions, activity modifications, home exercise programs, and strategies for pain management to empower active participation in the rehabilitation process and optimize recovery outcomes.
Compliance and Follow-Up
Adhere to prescribed rehabilitation protocols, attend scheduled therapy sessions, and communicate with healthcare providers to monitor progress, address concerns, and adjust treatment as needed throughout the recovery journey.