Significance of Pediatric/Adult Spasticity Management:
Comprehensive Assessment
Pediatric/adult spasticity management begins with a comprehensive assessment of the individual’s medical history, neurological function, musculoskeletal status, and functional abilities. Healthcare providers utilize standardized assessments, clinical evaluations, and diagnostic imaging to identify the severity, distribution, and impact of spasticity on the individual’s daily life and mobility.
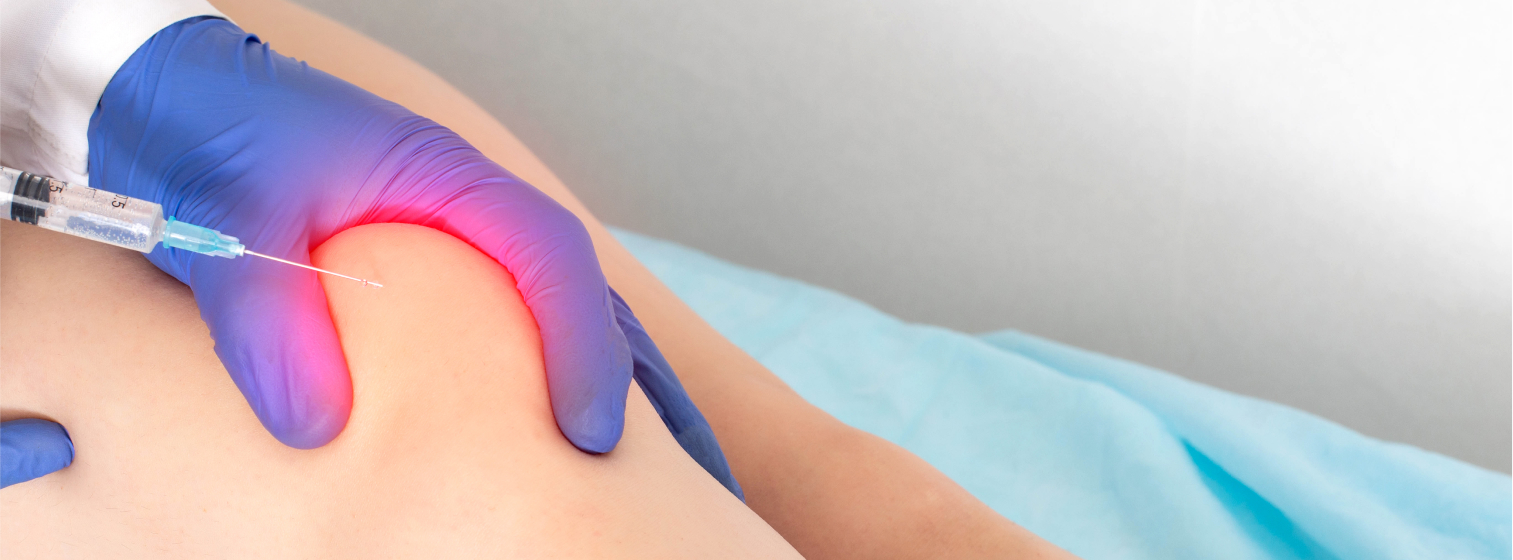
Multimodal Treatment Approach
Spasticity management encompasses a multimodal approach that combines pharmacological interventions, physical therapy, orthotics, assistive devices, and interventional procedures to address the complex needs of pediatric and adult patients. Treatment plans are tailored to the individual’s age, diagnosis, goals, and preferences, with the goal of improving motor function, reducing pain, and enhancing overall well-being.
Early Intervention
Early intervention is essential in pediatric spasticity management to minimize the impact of spasticity on motor development, musculoskeletal alignment, and functional outcomes. Healthcare providers collaborate with families, caregivers, and multidisciplinary teams to implement early intervention strategies, such as stretching exercises, positioning techniques, and orthotic interventions, to promote optimal motor development and prevent secondary complications.
Functional Improvement
Spasticity management aims to improve functional outcomes and quality of life for pediatric and adult patients by reducing muscle stiffness, improving range of motion, and enhancing motor control. Rehabilitation programs focus on functional activities, gait training, activities of daily living, and adaptive strategies to maximize independence and participation in meaningful activities.
Preventing Secondary Complications
Spasticity management addresses the prevention and management of secondary complications associated with spasticity, such as muscle contractures, joint deformities, pressure ulcers, and pain. Healthcare providers implement preventive measures, including range of motion exercises, splinting, seating and positioning modifications, and skin care interventions, to minimize the risk of complications and optimize long-term outcomes.
Holistic Care
Pediatric/adult spasticity management adopts a holistic approach to care that considers the physical, psychological, social, and environmental factors influencing the individual’s well-being and functioning. Healthcare providers collaborate with individuals, families, caregivers, and community resources to address the diverse needs and preferences of pediatric and adult patients and promote holistic health and wellness.
Approaches to Support Pediatric/Adult Spasticity Management:
Collaborative Care
Engage in collaborative care with a multidisciplinary team of healthcare providers, including neurologists, physiatrists, orthopedic surgeons, physical therapists, occupational therapists, and orthotists, to develop a comprehensive spasticity management plan tailored to the individual’s needs and goals.
Individualized Treatment Planning
Customize spasticity management interventions to meet the unique needs, preferences, and goals of pediatric and adult patients, considering factors such as age, diagnosis, severity of spasticity, functional limitations, and psychosocial factors. Involve individuals and their families in treatment planning and decision-making to ensure a patient-centered approach to care.
Evidence-Based Practice
Utilize evidence-based assessment tools, treatment techniques, and clinical guidelines in pediatric/adult spasticity management to ensure the effectiveness, safety, and quality of care. Stay informed about current research, best practices, and advancements in the field to optimize treatment outcomes and promote continuous quality improvement.
Family/Caregiver Education
Provide education and support to families, caregivers, and support networks regarding spasticity management strategies, home exercises, assistive devices, and community resources. Empower families to actively participate in their child’s or loved one’s care and advocate for their needs within healthcare and educational settings.
Functional Goal Setting
Collaborate with pediatric and adult patients to establish functional goals that are meaningful, achievable, and relevant to their daily lives and aspirations. Use goal-oriented interventions and outcome measures to track progress, celebrate achievements, and adjust treatment plans as needed to maximize functional improvement and quality of life.
Long-Term Follow-Up
Implement a long-term follow-up plan to monitor the ongoing effectiveness of spasticity management interventions, assess for changes in functional status or spasticity severity, and adjust treatment strategies accordingly. Provide continuity of care and support to individuals and their families across the lifespan, addressing evolving needs and transitions in care settings.